Nicolas Lefevre(1,2)*, Yoann Bohu(1,2), Jean François Naouri(1), Shahnaz Klouche(1), Serge Herman(1,2)
(1) Clinique du Sport, 36 boulevard Saint Marcel 75005 Paris, France
(2) Institut Nollet, 23 rue Brochant 75017 Paris, France
* Corresponding author
E-mail: secretrariat@chirurgiedusport.com
Phone: + 33 (1) 40 79 40 36
Introduction
While muscle injuries of the posterior region of the thigh are common in athletes, the proximal hamstring rupture is a rare disease. A study published in 2003 [1] analyzed in a consecutive series of 170 patients, 179 trauma hamstrings occurred over a period of 3 years. MRI and / or ultrasound showed that only 12% of the injuries were fractures of the proximal and 9% complete ruptures. It is also little known, the first cases described in the literature from 1988 [2]. Clinically the patients describe a violent pain in the buttock (stab printing) followed by leg weakness. Physical examination showed a large posterior hematoma and palpation found a void under the ischial tuberosity. The traumatic mechanism combining classic acute hyperflexion of the hip and knee hyperextension with a violent eccentric contraction of the hamstrings. MRI performed in emergency confirms the tendon rupture.
In 1996, Sallay [3] showed that Functional results were better after surgical repair with conservative treatment. Some patients are operated after failure of conservative treatment [4-7] and recovering a satisfactory function. Cohen [8] recommends surgery in case of tendon rupture or a displaced bone fragment of more than 2 cm, or in case of complete rupture. Surgery is now the rule, although some authors [9] describe clinical cases successfully treated with a simple medical treatment. This superiority of surgery was confirmed in a review of the literature [10] recently published.
It is also necessary to differentiate acute ruptures chronic ruptures, according to the time elapsed between trauma and surgical repair. Klingele [11] has set the limit at four weeks, at which time the surgery was becoming more difficult due to the formation of a beginning of fibrosis around the sciatic nerve. This technical problem has also been highlighted by other authors [12-14]. It is especially important to analyze these two groups separately as functional results seem better if surgical repair is before 4 weeks of evolution. [10]
However, the surgical technique is relatively new, difficult and requires a good anatomical knowledge of the ischial region.
Anatomy
Gluteal region and posterior femoral region
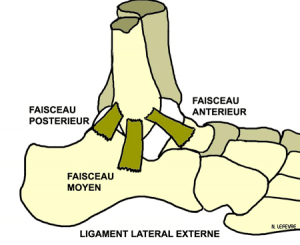
Located at the back of the hip, the buttocks is limited by the iliac crest on top, the greater trochanter and outside the gluteal fold down. Surgical point of view, it is important to note that the gluteal fold does not match the lower edge of the gluteus maximus but the cross obliquely (Fig.1).
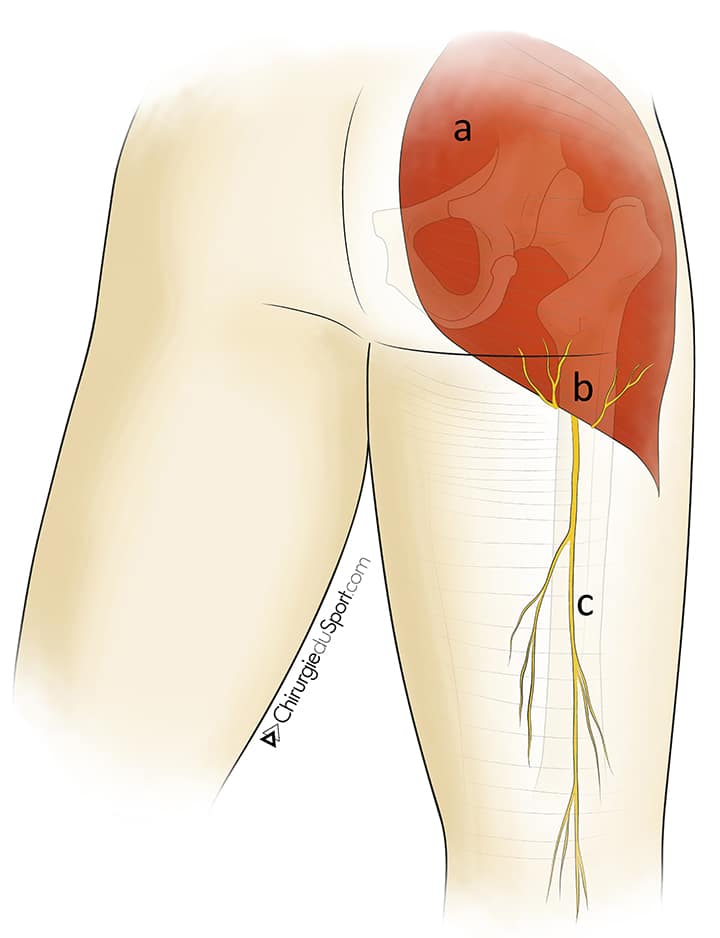
a- gluteus maximus.
b- cutaneous branch of the small gluteal sciatica.
c- cutaneous branch of the sciatic small.
In addition, in this region, in the thick and supple skin is a fatty layer, made ??of adipose platoons separated from each other by fibrous tract. The fiber spans of the subcutaneous fat layer is attached to the undersurface of the dermis and the underlying fascia. Surgical dissection of this area is more difficult because there is no superficial fascia. The gluteal cutaneous branch of the sciatic small and perforating cutaneous nerve cheminent within this fatty layer (Fig.1). .The fascia covering the gluteus maximus is fine, difficult to isolate surgically. The lower edge of the gluteus maximus is obliquely downward and outward, it crosses the horizontal gluteal fold. The gluteus maximus completely covers the ischium when the hip is in extension and discovered in hip flexion. This anatomical region is to know the way to horizontal surgical approach in the gluteal fold.
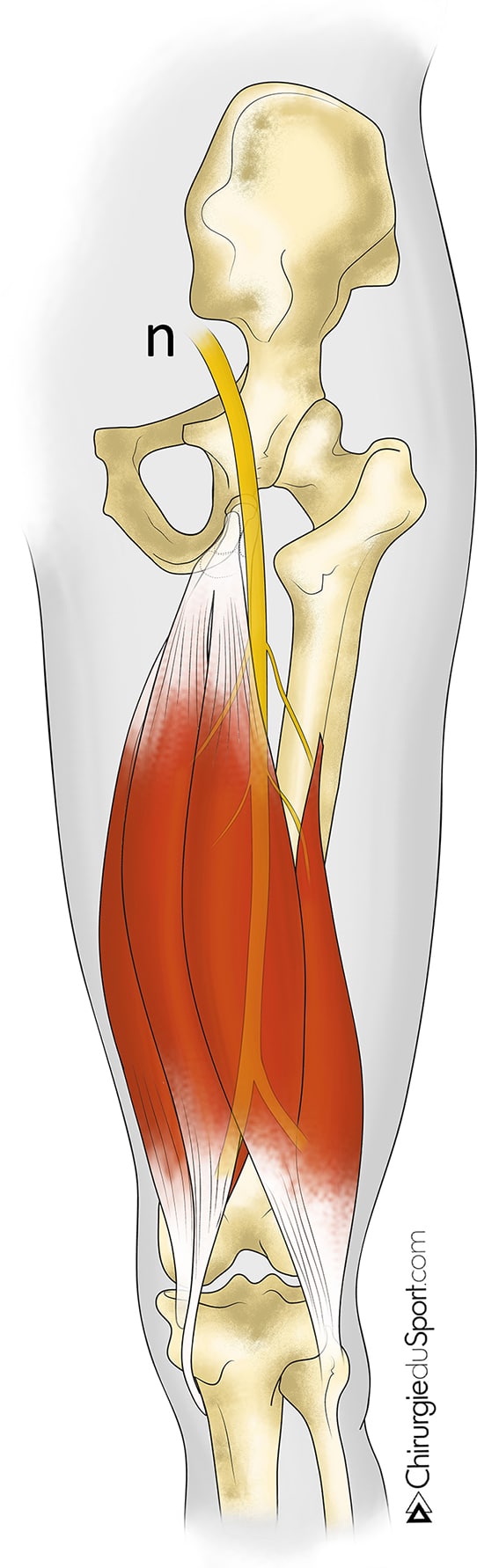
The posterior femoral region is the posterior part of the thigh in the gluteal fold. The subcutaneous tissue is separated from the deeper level by making superficial fascia dissection and the first in this region easier than in the gluteal region. Under this fascia travels vertically cutaneous branch of the sciatic giving small branches through the fascia (Fig.1). The first muscle layer is formed by the semitendinosus medially and the long head of biceps outside. It forms a common proximal tendon inserting on the posterior surface of the ischial tuberosity. The second deeper muscle layer is formed by the semimembranosus and the short head of the biceps (Fig.2). The proximal tendon of the semimembranosus is thick and fits outside the semitendinosus, biceps, it extends by a broad tendon membrane. The sciatic nerve is located in a cellulignin adipose tissue web vertically under these two muscle layers, passing up outside the ischial tuberosity and the middle part in front of the biceps. It gives the innervation of all the hamstring muscles (Fig.3).
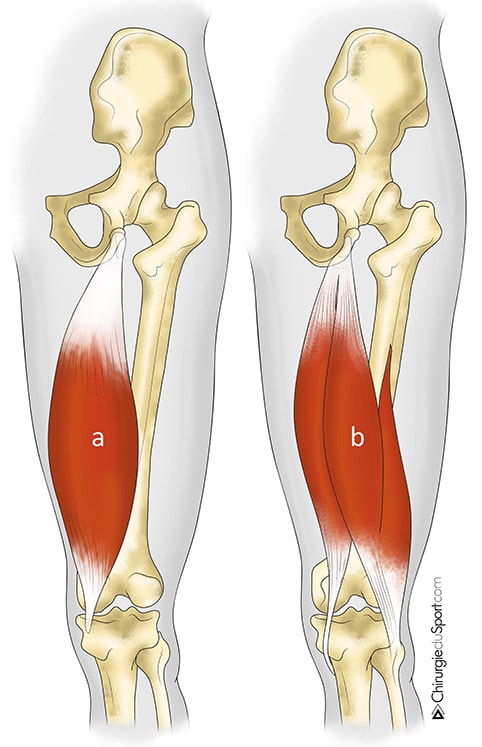
a- semimembranosus
b- semitendinosus muscle and biceps
with a common proximal tendon
The hamstring muscle group consists of three muscles of the posterior region of the thigh: the biceps femoris muscle (long head), the semitendinosus and semimembranosus. They fit up on the ischium and down on the tibia and the fibula head (Fig.2). These are important powerful muscles for standing, running, acceleration and braking. They are mainly flexors and secondarily leg extensors of the thigh. When walking or running, they are also antagonists quadriceps, slowing the advance of the leg at the end of the step and preventing the brutal and full knee extension. During the race, the hamstrings are subject to very high tensions. Their business interests more than 2/3 of the time of the complete cycle of the leg and is not limited to the back of the foot under the hip or front brake support. They are subject to various rhythms and contraction plans to cover the cycle of stride. They spend the concentric phase (back from suspension) to an eccentric phase in coordination with the quadriceps and braking in support of pre-support foot. They also have an important role in the striking of the ball (football). At the end of strikes, hamstrings hamperthe knee extension movement. This is an eccentric braking
Patients and Methods
A nonrandomized prospective single-center study compared non was conducted by the Sport Clinic Nollet Paris V and the Institute from January 2002 to July 2012 (10 years experience). Patients received full information and study obtained the favorable opinion of the Patient Protection Committee as non-interventional qu’étude.
Criteria for inclusion and exclusion
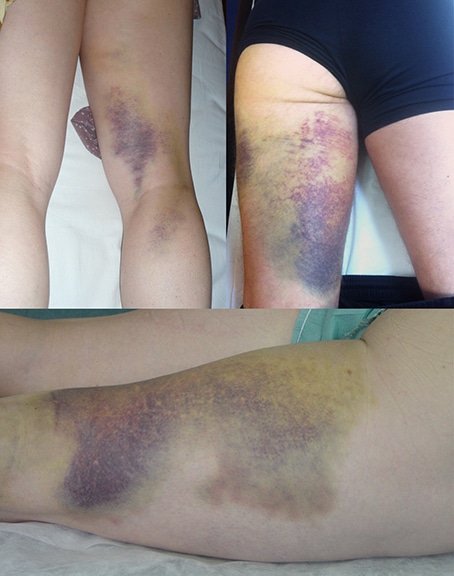
Inclusion criteria were (1) a partial or complete proximal hamstring rupture, (2) acute onset for less than 4 weeks and (3) treated surgically. The diagnosis of fracture was clinically referred to occurred after the trauma of a violent pain in the buttock, followed by leg weakness and a possible support, the formation of a hematoma posterior (Fig. 4) sometimes visible muscle retraction (Fig.5) and, upon palpation, vacuum the ischial tuberosity (Figure 6). The break was later confirmed by an MRI performed in emergency.


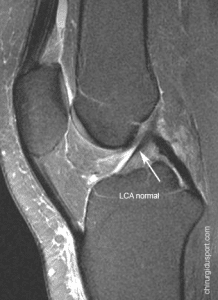
MRI
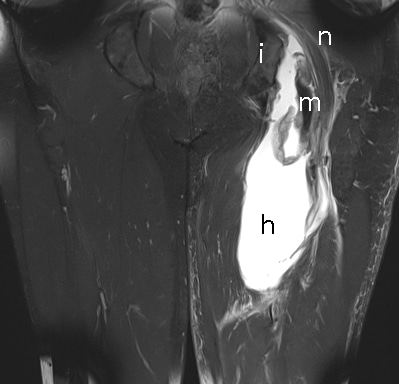
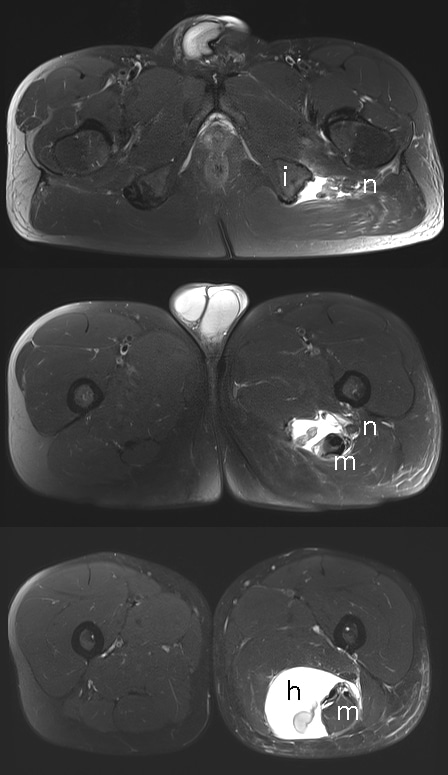
The MRI is the gold standard in the diagnosis of tendon ruptures hamstring. Using weighted sequences T1 and T2 Fat-sat (fat saturation) in the coronal plane (Fig.7) and axial comparatively antenna called “whole body”(Fig.8). A sagittal section plane in unilateral Fat-sat T2 sequence is sometimes useful. The field of study must be sufficiently large with full visualization of the ischium but the stump tendon ruptured, more or less retracted distally. MRI typically shows at the rupture site, a more or less substantial hematoma, variable signal as a function of delay from trauma. The retracted tendon stump, is found in the haem reshuffle with a typical appearance bell. The sciatic nerve is to be spotted throughout the height of the hematoma. Analysis of the MRI can diagnose partial or complete rupture of the tendon slides, appreciate the importance of tendon retraction (in cm) and the state of suffering and of the muscles trophicity
Surgical technique
Installation
The patient can be operated under general anesthesia or spinal anesthesia. The patient is installed in the prone position, the hip slightly flexed to 20 ° on a support, knee flexion of 60 ° on a knee bar (Fig.9). This installation can relax the hamstrings and allows easier reintegration without tension ruptured tendons.
First vertical track
In the case of a complete break with tendon retraction of more than 6 to 7 cm, we use preferably a way vertical first under the gluteal fold. A short vertical incision of 5 to 8 cm is made ??in the gluteal fold and plumb with the ischial tuberosity. It is not necessary to extend the incision horizontally in the gluteal fold (Fig.10). A first horizontal path in the gluteal fold is achievable for the retractions of less than 6 cm or partial tears.
After vertical opening of the superficial fascia, it individualizes the hamstring muscle group under the fascia usually surrounded by a large hematoma during resorption and creates a peel pouch for easy dissection. First you must locate the sciatic nerve, which travels outside and in front of the muscles in his fat (Fig.11). When the break is very recent (within 15 days), simply release the finger to distinguish and neurolyser the sciatic nerve. Sometimes a scarring start requires a true surgical neurolysis by releasing the tendon stump adherent to the sciatic nerve. Neurolysis This is necessary because we must avoid any traction nerve tendons during rehabilitation. After locating the nerve on the whole height of the incision, it is possible to rehabilitate tendons without risk to the nerve. It is not necessary to put the nerve Lake. Care must be taken not to damage the motor branches of the hamstrings.
Analysis of the tendon stump is not always easy but we must find the common tendon biceps tendon half backwards and inwards and half membranous tendon forward and off. Very often the three tendons are meeting in a periosteal flap avulsed flush with the ischial making it easier reintegration (Fig.12). The identification of the ischial tuberosity is difficult because the ischial deep and hidden under the buttock muscles, including the gluteus maximus. Must drag a valve under the gluteus maximus and spread it up and out. A freshening of the ischium with a rasp is necessary for proper healing tendons.
Transosseous the rehabilitation of tendons is performed using anchors or metal or absorbable and nonabsorbable son (DePuy Mitek, Norwood, Massachusetts). The use of metal anchors (Mitek GII SuperAnchor TM) requires a perfect visualization of the ischium, the anchor tunnel is drilled to the square tip and the anchor is attached under direct vision hammer. The GII anchors have a nonabsorbable suture set with a needle. The use of absorbable anchors (Mitek Anchor Lupine Loop TM) is easier. The ancillary TM Lupine Loop has a cannulated drill guide for drilling the ischium without damaging the sciatic nerve(Fig.13). After drilling the anchor to the engine tunnel, leave in place the cannulated drill guide and slide the anchor Lupine through the guide (Fig.14). The anchor is impacted with a hammer. Unlike GII anchors, Lupine Loop TM anchors are provided with two son unpressed. It is therefore necessary, before setting up the anchors, remove both son and put a nonabsorbable suture set with a needle (OrthocordTM Suture, DePuy Mitek, Norwood, Massachusetts) taking care of the needle to untwist it can pass into the chuck. There are two advantages to using Lupine anchors: they are absorbable, so there is less risk of disturbing secondary migration. Furthermore the mandrel protects the sciatic nerve and the soft parts in the tunnel drilling(Fig.14). There must be between 3 and 4 anchors in the ischium by the number of ruptured tendon. Crossing points in tendons are U-shaped with a double passage to block the wire in accordance with the 3 or 4 mounting areas.
The reduction and fixation of tendons are made ??by a simple pull of the wire free sliding in the anchor and can be traced back tendons as the “string up the sail on the mast of a ship”(Fig.15). The assembly is locked with simple nodes by successive half-rings. We must repeat this 3 or 4 times for a solid attachment of tendons. Then closing the superficial fascia and skin closure. A Redon drain is not systematic. In the operating room is placed a rigid splint fixed between 30 and 45 ° of flexion.
Route of the first horizontal gluteal fold
In the event of partial or complete break with little tendon retraction, a process of horizontal first in the gluteal fold is achievable (Fig.16 and 17). The postoperative appearance is certainly better (Fig.18) but dissection is more difficult and more limited vision. It is necessary to understand the anatomy of the region. The horizontal gluteal fold does not match the lower edge of the gluteus maximus but the cross obliquely. The incision is horizontal, you have to cross the fatty layer, made ??of adipose and fibrous platoons tract. then findthe gluteus maximus with its end fascia that covers it. It must then locate the lower edge of the gluteus maximus and lift with a valve to release the ischium. Dissection must be careful to avoid damage to the gluteal cutaneous branch of the sciatic small and perforating cutaneous nerve, causing secondary buttock dysesthesia (Fig.1).
Rehabilitation protocol
The protocol included three successive stages with different goals: healing, resume daily activities and the resumption of sporting activities. During the first week, the knee was immobilized with a simple splint in flexion to 30 ° to avoid tension on the suture. The support was partial with two crutches. The next five weeks, the splint was replaced by an articulated joint (Fig.19) permitting free knee flexion but a limited extension at 30 °. A gentle and progressive functional rehabilitation was started by an isometric work the quadriceps and hamstrings, knee flexed 30-45 °. The full support and seating position were allowed in the absence of pain. At the 6thweek, the knee was totally released with full support with and without poles. The active rehabilitation included a dynamic work the hamstrings initially helped by active and active against resistance and muscular work the quadriceps closed chain-type stepper. The patient could resume cycling with low resistance and a rapid cadence (80 rotations / min). During this phase, the therapy was started. Between 12 and 16 weeks, the patient resumed brisk walking and possibly a light jog. The muscle strengthening hamstrings isokinetic was continued, first by concentric and eccentric. Between the 16th and the 32nd week the resumption of regular sports activity was allowed.
Monitoring protocol patients
Postoperatively, patients were clinically evaluated at 6 weeks, 3 months, 6 months, 1 year and then every 3 years. An MRI control and isokinetic Biodex ® tests (Fig.20) were made ??a minimum decline of 6 months.
Outcome
The primary endpoint was the resumption of the sport. The secondary endpoints were the sports recovery time, the level of recovery, the duration of the work stoppage, the healing of tendons MRI monitoring, the report hamstring / quadriceps on the isokinetic tests and, last follow, the presence of residual pain and / or sciatica nerve block and a satisfaction questionnaire (very satisfied, satisfied, fairly satisfied, disappointed).
Patients
During this period, 60 patients were operated in the service for a total or partial rupture of proximal hamstring which 34 patients within 4 weeks of evolution. The series of acute ruptures were 9 women and 25 men, mean age 39.3 years (18 to 60). The right side was affected in 22 patients and left side in 12 patients. Two patients did not practice any sport, three were professional athletes, 12 were practicing competitive sport and recreational sport a 17. The traumatic mechanism was identical combining acute hyperflexion of the hip hyperextension of the knee with a violent eccentric contraction of the hamstrings. No direct trauma to the ischial tuberosity were reported. The break had occurred during a sports activity in 29 patients (85.3%) and following a domestic accident (slip) in 5 patients (14.7%) (Table 1). The movement was responsible for the injury forced the big difference (Fig.21) (rugby, fencing, running and sliding), a large acceleration (rugby, skeleton, water skiing) (Fig.22) or shoot into space (football) (Fig.23). All patients were referred directly to the service. The patients had various clinical signs of rupture of the hamstring (Table 2). Fifteen patients presented with an ultrasound carried out within an average of 3.7 days (from 1 to 7) showing a hematoma in all cases and evoking a partial rupture of the hamstring in 3 cases. The MRI was performed in an average 5.9 days (1 to 15) and confirmed the diagnosis of rupture in all cases.
The patients were treated surgically within an average of 13.6 days (range 5-30). The tendon rupture was complete in 23 patients (5 of periosteal avulsion) (Fig.24 and 25), partial for two tendons (Fig.26) (biceps and semitendinosus) in 7 patients and one tendon (Fig .27) (the semimembranosus) in 4 patients. The average shrinkage was 5.8 cm (2 to 10). The average number of anchors used was 3.4 (2 to 4) metal in 12 patients operated on before December 2007 and absorbable in 22 patients operated on after that date. Postoperatively, one patient had a large hematoma that required drainage in emergency evacuation. The MRI scan was actually performed in 19 (55.9%) patients at a mean of 15.8 months (range 6.2 to 86.2) and isokinetic tests in 17 (50%) patients with mean follow-up of 10.9 months (range 6.2 to 26.3). No iterative rupture occurred during follow-up. The average follow-up was 27.2 months (6 to 85.7) without any lost.
Results
All sports patients (32/34) resumed their activities within an average of 5.7 months (2.3 to 9.3), the same level for 27 patients (79.4%) and at a lower level for 7 patients (20.6%). Of the 15 athletes that had the series, 12 (80%) returned the sport at the same level. The duration of the work stoppage was an average of 3.2 months (1.2 to 8.1).
At a minimum decline of 6 months, the MRI scan showed a healing hamstring tendons in all patients (Fig.28). Isokinetic tests showed that the strength of the hamstring averaged 92.7% (from 68 to 127%), 93.8% (from 68 to 124%) and 100.8% (83 to 125% ) compared to the contralateral limb 90 °, 180 ° and 240 ° per second. The report hamstring / Quadriceps medium was 54.7% (41 to 74%) to 240 ° per second.
At last follow, 3 (8.8%) patients had discomfort or mild pain during prolonged sitting. One patient developed a hamstring tendinopathy following the migration of a metal anchor and for which he received a combing a decline of 71.5 months. No cases of sciatica nerve trunk was found.
Twenty-six (76.5%) patients were very satisfied, 4 (11.75%) satisfied, 4 (11.75%) moderately satisfied and none were disappointed by the response.
Discussion
In this study, surgical repair of acute fractures proximal hamstring allowed all patients to resume sports activities at the same level for most of them. The patients were very satisfied or satisfied large majority.
All patients resumed their sports activities at a mean of 5.7 months, 79% at the same level, which is comparable to what has already been published. Sallay [3] showed that after a single conservative treatment 58% of patients took up the sport. If surgical treatment, this rate varies between 76% [20] and 87% [7] in an average of 5 to 6 months. Athletes have taken the sport at the same level in 80% of cases. This rate was 74% in the series of Sarimo [15] and 87% for patients Lempainen [7]. Patients were very satisfied to satisfied in 88.2% of cases which is also comparable to the literature.
Isokinetic tests showed that the ratio hamstrings / quadriceps was 54.7% (41 to 74%) in average. Brucker [16] found an average ratio of 55% (from 44% to 66%).
In this series, there were no cases of recurrent tears and at last follow no patient had sciatic or disabling pain. These complications are most often observed in chronic failure [10,17]. In the study of Sarimo [15], an iterative rupture covered five patients (12.2%) including a series of acute and chronic ruptures.
Metal anchors were replaced with absorbable anchors in December 2007 because one patient developed a hamstring tendinopathy following the migration of a metal anchor. The development of a specific ancillary encouraged surgeons to change the method. No complications were noted due to this change in method of attachment.
The study also shows that this condition does not occur during a sporting activity, five patients with ruptured hamstring after a domestic accident slip types. Rugby was the most frequently offending sport. For Wood [18], he was waterskiing but this is probably due to a selection bias.
The main strengths of this study were first its prospective nature with which we have no lost. Most published studies were retrospective with a number of important lost sight of. Furthermore, this study analyzed only acute ruptures and this is one of the largest series. Indeed series Bucker [18] included acute ruptures 6 out of 8 patients, Series Birmingham [19] 9 of 23 patients evaluated, the study Sarimo [15] 14 acute ruptures of 41 and Folsom [20] 21 acute in a series of 26 patients.
One weakness of the study was the lack of a “conservative treatment” group. But, with the results published in the literature, it does not seem ethical to offer medical treatment to the patient.
Conclusion
Surgical repair breaks acute proximal hamstring has significantly improved the functional outcome of patients but it remains a serious disease that can jeopardize their sporting future. It must be diagnosed and repaired as soon as possible to avoid loss of therapeutic opportunity.
Declaration of interest
The authors declare that they have no conflicts of interest related to this article.
Thanks
Our thanks to Mr Mathieu Pinet for illustrating the article.
References
1. Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32(10):582-9.
2. Ishikawa K, Kai K, Mizuta H. Avulsion of the hamstring muscles from the ischial tuberosity: a report of two cases. Clin Orthop Relat Res. 1988 ;232:153–155.
3. Sallay PI, Friedman RL, Coogan PG, et al. Hamstring muscle injuries among water skiers. Functional outcome and prevention. Am J Sports Med 1996;24:130–136.
4. Chakravarthy J, Ramisetty N, Pimpalnerkar A, Mohtadi N. Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders: a report of four cases and review of the literature. Br J Sports Med. 2005;39(8):569-572.
5. Cross MJ, Vandersluis R, Wood D, Banff M. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. Am J Sports Med. 1998;26(6):785-788.
6. Kirkland A, Garrison JC, Singleton SB, Rodrigo J, Boettner F, Stuckey S. Surgical and therapeutic management of a complete proximal hamstring avulsion after failed conservative approach. J Orthop Sports Phys Ther.2008;38(12):754-760.
7. Lempainen L, Sarimo J, Heikkila J, Mattila K, Orava S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med 2006;40:688–691.
8. Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15(6):350-355.
9. Kraus TM, Siebenlist S, Sandmann G, Stöckle U, Elser F. Non-operative treatment of complete rupture of the proximal hamstring tendons. Acute functional and radiologic assessment with 3-month and 2-year follow up. Injury Extra (10 September 2009) doi:10.1016/j.injury.2009.08.012
10. Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures: a systematic review. Int J Sports Med. 2011;32(7):490-5.
11. Klingele KE, Sallay PI. Surgical Repair of Complete Proximal Hamstring Tendon Rupture. Am J Sports Med. 2002 ;30 :742-747.
12. Carmichael J, Packham I, Trikha SP, Wood DG. Avulsion of the proximal hamstring origin. Surgical technique. J Bone Joint Surg Am. 2009;91(S2):249-256.
13. Hernesman SC, Hoch AZ, Vetter CS, Young CC. Foot drop in a marathon runner from chronic complete hamstring tear. Clin J Sport Med. 2003 ;13(6):365-368.
14. Orava S, Kujala UM. Rupture of the ischial origin of the hamstring muscles. Am J Sports Med. 1995;23(6):702-705.
15. Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med. 2008;36(6):1110-1115.
16. Brucker PU, Imhoff AB. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):411-418.
17. Carmody C, Prietto C. Entrapment of the sciatic nerve as a late sequela of injury to the hamstring muscles. A case report. J Bone Joint Surg Am. 1995;77(7):1100-1102.
18. Wood DG, Packham I, Trikha SP, Linklater J. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90(11):2365-2374.
19. Birmingham P, Muller M, Wickiewicz T, Cavanaugh J, Rodeo S, Warren R. Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am. 2011;93(19):1819-1826.
20. Folsom GJ, Larson CM. Surgical treatment of acute versus chronic complete proximal hamstring ruptures: results of a new allograft technique for chronic reconstructions. Am J Sports Med. 2008;36(1):104-109.
| Activity during the trauma | Number of patients |
| Rugby | 6 |
| domestic accidents | 5 |
| Jogging | 4 |
| Soccer | 3 |
| water ski | 2 |
| Tennis | 2 |
| Aikido | 1 |
| Badmington | 1 |
| Canyoning | 1 |
| Cycling | 1 |
| Climbing | 1 |
| Fencing | 1 |
| Handball | 1 |
| Karate | 1 |
| Skeleton | 1 |
| Ski | 1 |
| Squash | 1 |
| Volleyball | 1 |
| Clinical signs | Number of Patients (%) |
| feeling – creak – slam – Tear – None of the three | 13 (38.3) 5 (14.7) 5 (14.7) 11 (32.3) |
| Stab in pain when trauma | 15 (44.1) |
| Pain intensity during the trauma – syncopale – Strong – Average | 5 (14.7) 25 (73.5) 4 (11.8) |
| Pain intensity in the sitting position during admission – Strong – Average – Low – Any | 15 (44.1) 11 (32.3) 4 (11.8) 4 (11.8) |
| Sciatica when admisssion – Any – Low – Average | 30 (88.2) 2 (5.9) 2 (5.9) |
| posterior hematoma – Important – Way – Small | 19 (55.9) 7 (20.6) 8 (23.5) |
| Muscular weakness – important – Average – Low | 21 (61.8) 12 (35.2) 1 (3) |
Figure legends
Fig 1: anatomy of the posterior femoral gluteal and thigh region. Sensory innervation of the buttock and thigh.
a) gluteus maximus b) gluteal cutaneous branch of the small sciatic c) cutaneous branch of the small sciatic
Fig 2: The muscle group hamstring
a) semi-membranous muscle b) semitendinosus muscle and biceps tendon with a common proximal
Fig 3: Reports of muscle group hamstring with the sciatic nerve
Fig 4: post-traumatic hematoma after proximal complete rupture of the hamstring tendons
Fig 5: Complete rupture of the proximal hamstring tendons 3 with muscle retraction.
Fig.6: palpation of a vacuum under the ischial tuberosity
Fig 7: MRI T2-weighted sequences Fat-sat (fat saturation) in the comparative coronal plane antenna called “whole body” complete visualization of the ischium (i) of the tendon stump broken retracted distally (m) of the large hematoma (h) and sciatic nerve (n)
Fig 8: MRI T2-weighted sequences Fat-sat in the comparative axial plane. Complete visualization of the ischium (i) of the tendon stump broken retracted distally (m) of the large hematoma (h) and sciatic nerve (n)
Figure 9: Installation on operating table in the prone position and a single tap (knee bar) below the ankle
Fig 10: First vertical Way under the gluteal fold to break a proximal hamstring tendons with tendon retraction of more than 6 cm.
Fig 11: Nerve (n) in contact with the muscle hamstring (m)
Fig 12: Complete rupture of the proximal 3 tendons with avulsion of a periosteal flap
Figure 13 Drilling bone tunnels with Lupine chuck ™
Figure 14: Inserting the anchors through the mandrel Lupine ™ guide
Fig 15 Passing son and traction as the “string up the sail on the mast of a ship”
Fig 16 first horizontal Way posterior in the gluteal fold
Figure 17 Route of horizontal first to break with proximal tendon retraction under 6 cm
Fig 18 first road in the crease of the buttocks, aesthetics
Fig 19 Immobilization in a hinged knee brace
Fig 20 Test Biodex®
Fig 21: Large gap forced with maximum stretch the hamstrings
Fig 22 out acceleration or waterskiing
Fig 23 Shoot into space
Fig 24 proximal Complete rupture of the three tendons
Fig 25 proximal Complete rupture with periosteal flap
Figure 26: Out of two tendons: the biceps tendon and the half
Fig 27: Ruptured tendon half membranous
Fig 28 control MRI at 6 months of a complete break proximal hamstring.:
MRI T2-weighted sequences Fat-sat (fat saturation) in the comparative coronal plane antenna called “whole body” complete visualization of the ischium (i) of the tendons healed (m), and visualization of the anchors in the ischium ( at)
MRI T2-weighted sequences Fat-sat in the comparative axial plane. Complete visualization of the ischium (i), and tendons healed
Doctor Nicolas LEFEVRE, Doctor Yoann BOHU, Doctor Antoine GEROMETTA, Doctor Shahnaz KLOUCHE , Doctor Serge HERMAN. – 18 septembre 2015.