Introduction
An update on this surgery is necessary because the quality of the results is based on a rigorous in the indication, the choice of the prosthesis, and surgical technique.
After a difficult start in the 70s, the precursors are Insall J. and M. Freedman, considerable progress has been made with the best knowledge of the anatomy of the knee remains and its biomechanics.
The improved design of the prosthesis, its integration into the ligament balance and the quality of materials has helped to make this reliable surgery.
CLASSIFICATION AND CHOICE OF IMPLANTS
The prostheses are divided into three classes:
1. Unicompartmental
2. bicompartmental
3. tricompartmental
Not a constraint
b Semi constraint
c Constraint

1. uni-compartmental prostheses
The uni-compartmental prosthesis replaces the joint surface of one internal or external compartment. Resurfacing is limited to the injured compartment without touching the ligaments or other compartments must be healthy. It can also integrate the patellofemoral prosthesis in this classification.
2. bicompartimentales prostheses
Many first generation total hip knee were designed and intended to replace the two articular surfaces of the femur and tibia without replacement of the patellofemoral joint patellar quickly but given the poor results obtained with bicompartimentales, prostheses were designed to tricompartimentales be.
3 tricompartimentales prostheses
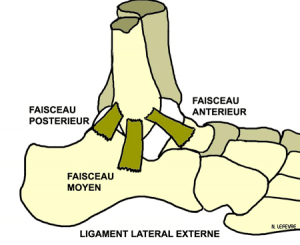
We must separate the slip aids more or less constraints depending on whether it meets one or both cruciate ligaments hinges prostheses (constraints)
The principle is a replacement of the three joint surfaces with a metal femoral condylar prosthesis which is based on a tibial tray and a medallion polyethylene patellar also polyethylene.
There are three types of sliding prosthesis (with fixed or movable plate)
a has the unconstrained prostheses
The unconstrained prostheses: it is a “resurfacing” of the three articular surfaces with preservation of all ligaments of the knee, including the cruciate ligaments. This is the only prosthesis that can restore normal knee kinematics (2) but it is rarely used because technically difficult and that in 40% of cases, the anterior cruciate ligament was gone.
Prostheses preservation of the posterior cruciate ligament: the stress of the two prosthetic components is minimal, respect the LCP allows the rotation sliding rolling movement by opposing posterior translation of the tibia in flexion.
The trays are less congruent without central cam.
b Semi-constraints prostheses
b Semi-constrained prosthesis: the design of implants (concave plate) provides stability to the knee. Resection of the posterior cruciate ligament requires intercondylar cam having a rear abutment effect in bending (6). Currently more and more of these prostheses are designed without cam but with a concave plate with polycentric sagittal radius (ultracongruentes prostheses)
c constraints prostheses
The constraints prostheses: prostheses hinges
Genuine hinges, they consist of two tibial and femoral elements having an elongated intramedullary rod and a pin system (bearing) permitting flexion-extension movements. (Cheetah Group 1970) Most Recent evolved allowing thanks to a double pin system to have movements of flexion-extension and rotation (semi-hinge prosthesis and pivot).
They have a number of disadvantages:
High bone sacrifice
Risk of fat embolism at the time of sealing (intraoperative shock)
Risk of sepsis operative largest post.
But especially high rates of loosening and fractures related to the importance of the stresses indicated at the stems.
corrosion problems (metal bearings) and wear (polyethylene bearings) at the axis (1,3).
These prostheses are however indicated for the treatment of bone tumors or bone or ligament major destruction (prosthetic recovery)
The mobile plates:
The mobile plates: for over 20 years now appeared the mobile-bearing prosthesis with or without conservation of the Crusaders. They have an anteroposterior translation movement, rotation, or mixed. Currently the most used mobile prostheses are ultracongruentes to pure axial rotation. It seems that the mobility of the insert reduces stresses at the interfaces and therefore polyethylene wear. (13)
Prostheses recovery
resumption of dentures, it is most often slip prosthetic posterior stabilized with the addition of intramedullary rods of varying length to ensure bone stability. Use of metal shims adapted to prosthetic systems to fill bone defects and sometimes bone grafts.
FIXING THE IMPLANTS
Two techniques: cemented and uncemented prostheses
Cemented prostheses:
The cement is an acrylic resin of polymethyl methacrylate. Its polymerization in minutes, makes an almost immediate holding of the prosthesis.
Prostheses without cement:
The primary coupling between the prosthesis and the bone is by impaction, the secondary bonding is a bone growth in contact with the implant through surface irregularity or an osteoconductive coating promoting regrowth bone (hydroxyapatite).
This requires a good quality bone with a perfect fit.
Currently the tendency is to associate a femoral component with cementless tibial components and cemented patellar (denture)
Knee osteoarthritis:
Primary or secondary knee osteoarthritis is the most frequent indication for total knee arthroplasty.
When osteoarthritis affects only a single compartment, the total prosthesis is not always indicated.
Indeed, internal knee tibiofemoral in a young patient with varus must discuss a tibial valgus osteotomy. When the indication is well put, it provides more than 80% good result in 10 years.
We can also offer a unicompartmental (PUC) in older sedentary subjects as are simpler in general, with early recovery support. (22)
Isolated patellofemoral osteoarthritis is difficult to treat, because the results of femoro patellar prosthesis while encouraging are excellent, now more teams propose to do from the outset a total knee replacement with a better result.
In all cases the indication of PTG is asked after a well conducted medical treatment (analgesics, anti-inflammatory, infiltrations, visco-supplementation, joint lavage) or conservative surgery (osteotomy)
Rheumatoid arthritis:
Rheumatoid arthritis:
Involvement of the knee is rarely isolated and within the scope of polyarthritis in fragile patients. The indication may be put to the inflammatory stage or stage effects. We must quickly make these patients before major bone destruction as surgery becomes more difficult with massive use of implants, bone grafting may even hinge prostheses.
The aim is to restore the patient indolence and early independence among these often multi operated patients.
Other inflammatory rheumatic diseases:
Rarer, they have the same indications.
Necrosis:
It most often affects the internal condyle, it is a good indication of a PUC, but only if the necrosis is not extended. Otherwise, it is preferable to perform TKA immediately because the risk of loosening of the femoral implant is indeed important in bone necrosis being poor.
We must discuss osteotomy in young subjects.
Tumors:
The management should always be done in a specialized center by a multidisciplinary team. It generally comprises the use of a hinge prosthesis allowing large tumor resections sometimes involving the use of massive allograft for bone reconstruction.
PREOPERATIVE ASSESSMENT
It must be comprehensive local and general:
A clinical examination is necessary to evaluate the mobility of the knee ligament knee condition, the trophic status of the lower limbs (skin and venous statements).
The imagery will include :
- radiography charge opposite knee and incidence of Schuss,
- a lateral view at 30 ° of flexion,
- an axial view of the ball to 30 ° of flexion,
- a goniometry face of the assembly of both lower limbs
- to evaluate the mechanical axis of the member.
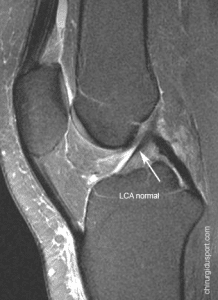
Sometimes a frontal radiograph for correction of the deflection position (stress valgus or varus) is useful. In contrast MRI is not indicated.
In the overall assessment, evaluation of cardiovascular status is essential, as well as research and eradication of all urinary including outbreaks. Following the general balance, anesthesia consultation will determine the type of anesthesia (ARL or AG) and the interest or not of autotransfusion.
INTERVENTION
It is carried out in an operating theater of prosthetic orthopedic surgery with a laminar flow or ventilation “class system 100” (number of particles in a cubic meter of air) while a “class system 1000” is sufficient for arthroscopy.
The member is washed, shaved, disinfected with betadine and surrounded by barren fields.
The procedure is done most often in the shoulder.
Various bone cuts are made using instrumentation suited to the chosen prosthesis (ancillary equipment), we must ensure the ligament balance and if necessary make releases (release) rarely ligament retentions.
Currently more and more prostheses are provided with a computer-ancillary equipment. The surgeon remains the operator but not the guide computer not in these bone cuts. The principle is to reconstruct a three-dimensional image of the operated knee and through a fixed sensor system temporarily on the knee, the computer guide into space carrying the surgical procedure.
This system is not widespread and ongoing evaluation.
OPERATIVE

Antibiotic prophylaxis is started in the operating room before inflation of the tourniquet and continued for 48 hours postoperatively. A drain by drain is left for 2 to 3 days. Some teams are introducing catheters femoral allowing a painless early rehabilitation.
Rehabilitation is started the next day with mobilization of the knee (manual or Kinetec). Sunrise is allowed the 2nd or 3rd day with full support with two crutches.
The patient comes to the 12th day. Rehabilitation continues for several weeks in center then domicile.En general flexion reached 90 ° between the 10th on the 30th day. When flexion is very limited at day 21, a mobilization under general anesthesia may be recommended. The patient was seen in consultation for a radiological assessment at 6 weeks and 3 months, 6 months, 1 year and then every 2 years.
COMPLICATIONS
GENERAL
thromboembolic
Probably underestimated because often asymptomatic (14, 15), their impact remains weak in the absence of major risk factors (obesity, venous insufficiency, phlebitis antecedent) A routine prophylaxis should be started by low molecular weight heparin, a lift early and wearing compression stockings postoperatively.
haemorrhagic
The postoperative blood loss can be significant, they are limited by a collector drainage system (cell sever) or compensated by the auto transfusion.
fat embolism
They are exceptional, and are described above at the time of sealing the long-stemmed prostheses. (Cheetah prosthesis)
COMPLICATIONS
locoregional
EARLY
Haemarthroses and haematomas
Hemarthroses and bruises are not uncommon and are relieved by the “icing” on the operated limb. They are bulky, it may be necessary to puncture the see of evacuating surgically.
Skin necrosis and disunity,
Skin necrosis and disunity, can involve becoming the prosthesis underlying. If limited attack, evolution is usually favorable after discontinuation of rehabilitation and wound care. However, they can sometimes require a surgical procedure (new suture) or a plastic gesture (covering flaps).
nerve paralysis
nerve paralysis are very rare (stretching the peroneal nerve after a large reduction or valgus knee flexion)
infectious
The risk of infection is a rare but serious complication that usually requires further surgery (to clean the operated joint and sometimes change the prosthesis) and a prolonged antibiotic therapy.
The infection rate is about 2%, this risk increases on certain lands (rheumatoid arthritis 8% (4), corticosteroids, diabetes) or during reoperation.
Infection can occur early (acute infection) before the 3rd postoperative week, it is due to contamination of the surgical site, usually through the skin.
It can be sub-acute (occurring within two years) or late in these cases it is most often blood-or lymphatic contamination from an infected site remotely.
It is essential to make the diagnosis early in order to achieve an appropriate and effective treatment. Clinical (fever, pain and local signs), biology (ESR, CRP), bone radioleucoscintigraphy and especially the joint aspiration to isolate the germ allow to confirm the diagnosis. (7)
The treatment always combines surgery and prolonged antibiotic therapy.
In the acute infection debutante washing synovectomie debridement of the knee without changing the prosthesis can allow healing.
In other cases the removal of the prosthesis is indispensable.La new prosthesis can be re-implanted in the same surgical time or distance after the biology of normalization. (5)
COMPLICATIONS
locoregional
LATE
Stiffness
Stiffness is a flexure limiting less than 90, it is often insufficient post operative rehabilitation or stopped. Early mobilization under general anesthesia with continued therapy allows in most cases to recover mobility.
The algo-neuro-dystrophic syndrome
The algo-neuro-dystrophic syndrome is rare, it requires prolonged medical treatment
fractures
The fractures are rare and usually traumatic. Intraoperative fractures are exceptional and are favored by osteoporotic bone.
Instabilities and dislocations
Instabilities and knee dislocations are the result of poor ligament balance or malposition of the implants. They may require further surgery.
usury
The wear of the prosthesis is the long-term major complication It is inevitable.
It has long asymptomatic.
It is, by the release of wear particles, causing an inflammatory reaction with peri prosthetic osteolysis responsible for loosening.
loosening
The loosening may be secondary to osteolysis peri-prosthetic or excessive constraints (hinge prosthesis or implant malposition) resulting in the onset of pain and a clear radiological border at the bone-implant interface. An early loosening must always check for infection. The migration of implants required revision surgery (RPTG);
CLINICAL RESULTS
The results of the different series are difficult to analyze. The evaluation criteria are not the same. Survival curves are usually as failure criterion, the prosthetic replacement and not loosening or wear.
However, analysis of published results showing survival curves between 93.5% and 96.8% at 15 years and recent studies (11 August 12) show a survival rate of between 90.77% and 93 6% at 20 years. (9 10). In the study of Insall, at 21 he has a survival rate of the prosthesis of 90.77% and the failure rate is independent of age, pathology requires that the prosthesis and finally weight. (10)
Over 90% of patients with total knee prosthesis have a satisfactory function at 15, ie a painless knee and an upper 90 ° flexion.
Pain is the main criterion in the result of a prosthesis, in 90% of cases the knee is painless (occasionally presence of some climatic pain (30%) do not require the taking of analgesic) in 10% of cases pain is most important and justifies a simple medical treatment.
Mobility is the second test, the recovery of the mobility is good and the various publications show a recovery of an average flexion of about 120 °. (12)
The patient with a knee replacement can have a normal daily life with a walk without a cane without limitation of distance and sometimes take reasonable sports physical activity (walking, swimming, cycling, golf …)
Polyethylene wear
The wear of the prosthesis is the major long-term complication. The use of polyethylene as the sliding interface in the prostheses is universal, unlike the hip where use of another friction torque (metal-metal, alumina-alumina).
Improving the quality of polyethylene (purity, high density) and sufficient thickness> 8 mm limit wear.
the edgings
The problem of radio-transparent border in sealed knee replacement is
probably overestimated; many authors failed to demonstrate any
correlation between the existence of a border, its progression, and clinical outcome.
Usually these radiolucent lines appear quickly and rarely progress.
Reversals
If loosening shelf wear without a recovery with change of the polyethylene insert is a simple procedure which suites give excellent results.
However in case of loosening with migration of implants, reoperation is often difficult because bone damage and deformation. It uses modular implants with intramedullary rod and metal shims to fill bone loss. Sometimes the use of bone grafts is necessary or even hinges prostheses.
mobile plate or not?
Total prosthesis mobile-bearing knee has a lifespan equivalent to that of PTG fixed shelf. It seems that the mobility of the insert reduces stresses at the interfaces and therefore polyethylene wear. (13)
The only complications that can be specifically attributed to the mobility plateau are dislocations of the insert or femorotibial dislocations.
PCL retaining or not?
The border tibial rate appears lower with prostheses PCL preservation. Indeed, Ewald (17) and Laskin (18) relate always less than 30 percent. 100, while Huten (19) and Insall (20) found 40 p. 100 and over edges. However Stern and Insall (20 21) recently reported a 94 percent survival rate. 100-12 years very reassuring as to the influence of the substitution of LCP on the longevity of the tibial sealing.
Finally we believe it does not seem to medium clinically significant argument
term advocating conservation LCP, especially as the surgical technique is more difficult.
CONCLUSION
Advances in design, materials and installation techniques for knee prostheses have helped make this safe and reliable intervention Long-term (20 years). With recent models of excellent result is obtained, the knee is stable, mobile and painless.
Nevertheless, it remains delicate surgery, and requires great rigor in the indication, the choice of implant and surgical technique.
BIBLIOGRAPHY
1 Aubriot JH, Huten D, Ph Hernigou, Pelisse F Marie F, knee prostheses. In: Design of joint prostheses, education notebook SOFCOT. Paris: French Scientific Expansion 1993; 44: 91-140
2 Stiehl JB, Komistek FD, JM Cloutier, Dennis DA, The cruciate ligament in total knee arthroplasty: a kinematic analysis of 2 total knee arthroplaties. J Arthroplaty. Aug 2000; 15 (5): 545-50
3 Mascard E, P Anract, Touchene A Pouillard P Tomeno B, Complication from the hinged Guepar prosthesis after-rescetion of knee tumor. Rev Chir Orthop 102 cases in 1998; 84 (4): 628-37
Laskin RS 4: Total condylar knee replacement patients in Who-have RA A ten year follow-up study. J Bone Joint Surg 72 A: 529-535, 1990.
5. Matthew M. infected total knee replacements. In: SOFCOT teaching Workbook. Paris: French Scientific Expansion 1995; 52: 51-61
6. INSALL JN, LACHIEWIECZ FP, Burstein AH: The posterior stabilized
condylar prosthesis. J Bone Joint Surg (Am), 1982, 64, 1317.
7. Tsukayama DT, Golderberg VM, Kyle R, Diagnosis and management of infected total knee arthroplasty after-. J Bone Joint Surg 2003; 85-A Suppl 1: S75-80
8 Vazquez-Vela G Johnson, Worland RL, J Keenan, Norambuena N: Patient demographics as a predictor of the ten-year survival rate in primary total knee replacement. J Bone Joint Surg 2003 (Br) in January; 85 b (1) 52-6
9 Rodriguez JA, Bhende H, Ranawat CS: condylar total knee replacement: a 20-year followup study.Clin July Orthop 2001; (388): 10-7
10 Font-Rodriguez DE, Scuderi GR, Insall JN: Survivorship of cemented total knee arthroplasty. Clin Orthop 1997 December; (345): 79-86
11 Ritter MA, Berend ME, Meding JB, Keating EM, Faris PM, Crites BM Long term followup of AGC PCL Retaining total knee replacement Clin Orthop 2001 July (388): 51-57
12 Hoffman AA Evanich JD Ferguson RP, Camargo PM: Ten to 14 year clinical followup of cementless knee natural system Clin Orthop (388) July 85-94
JN 13 argenson O’Connor JJ: polyethylene wear in meniscal knee replacement J Bone Joint Surg 1992 March 74 B (2) 228-232
14 Grady_Benson JC, Oishi CS, Hanson PB, Colwell CW Jr, Otis SM, Walker RH; Post operative monitoring for deep venous thrombosis with duplex ultrasonography after-total knee arthroplasty. J Bone Joint Surg 1994 A 76 (11) 1649-1657
15 Berry DJ; Monitoring for venous thromboembolic disease after-total knee arthroplaty. Clin Orthop 2001 Nov (392): 257-66
16 AJ Price, Rees JL Beard D, Juszczak E, Cater S, White S, R De Steig, Dood CA, Gibbons M, Mc Lardy-Smith P, Goodfellow JW, Murr DW; A mobile-bearing total knee prosthesis Compared with a fixed bearing prothesis. A multicenter single-blind randomized controlled trial. J Bone Joint Surg Br 2003 January; 85 (1): 62-7
17. Ewald FC, MA JACOBS, Miegel RE: Kinematic total knee replacement. J Bone
Joint Surg (Am) 1984, 66, 1032-1039.
18. LASKIN RS: total knee arthroplasty RMC. J Arthroplasty 1986, 1, 91-98.
19. hüten D DUPARC J: Implant tricompartmental Freeman and Mark II
Samuelson. Cahier teaching SOFCOT 35, 69-82 Scientific Expansion
French, Paris, 1988.
20. JN INSALL, MOOD RW Flawn LB DJ SULLIVAN: The total condylar knee
prosthesis in gonarthrosis. A five to nine year follow-up of the first one hundred consecutive
replacements. J Bone Joint Surg (Am) 1983, 65, 619-628.
21. STERN HS INSALL JN: Posterior Stabilized Prosthesis. Results after-follow-up of
nine to twelve years. J Bone Joint Surg (Am) 1992, 74, 980-986.
22; Witvoet J, Peyrache MD, Nizard RS. unicompartimentaires knee prostheses like lotus in the treatment of knee osteoarthritis lateralized. Results de135 cases with a mean of 4.6 years. Rev Chir Orthop 1993; 79: 565-76.
Doctor Nicolas LEFEVRE, Doctor Yoann BOHU, Doctor Serge HERMAN. – 7 octobre 2012.