Doctor Yves Guglielmetti
Sport Clinic -Paris
summary
The use of PRP has become widespread in sports trauma for the last decade, as an alternative to surgery or as a surgical adjuvant. High-profile successes in high-level athletes, and the abolition of the list of substances and methods prohibited by WADA at the end of 2010, have literally sparked the appeal for this technique.
The absence of side effects and excellent tolerance, make the injection of PRP, carried out under rigorous conditions, a technique ofGreat safety .
In our current state of knowledge, the efficacy of PRP therapy is no longer demonstrated in the treatment of cartilage lesions (7 studies with a high level of evidence), which is superior to hyaluronic acid.
Ultrasound guidance and good pain management (analgesia of pallium 1 or 2, MEOPA) are essential in the injection of tendon and muscular lesions but rarely necessary in the painful joint injection.
Treatments vary greatly from one practitioner to another, in terms of platelet concentration, cell richness (erythrocytes, leukocytes), ultrasound tracking, pain management, number of sessions and accompaniment. It is essential to better define the protocols through comparative studies.
The rehabilitation phase and workout reconditioning is an essential step, often overlooked when the PRP is presented as a miracle cure!
History of Platelet Concentrates
PRP platelet concentrates are the origin of blood derivatives used in hematology for the prevention and treatment of haemorrhages due to severe thrombocytopenia of central origin.
Platelet concentrates used as surgical adjuvants and then in sports traumatology were arbitrarily referred to as PRP as the standard platelet concentrates of transfusion hematology.
According to hardware manufacturers and authors,Different terms are used to define these platelet concentrates: PRP ( Platelet Rich Plasma) , cPRP (concentrated PRP), PRGF (Plasma Rich in Growth Factors), autologous blood . We will see that these concentrates are variable in their composition, in terms of concentration of growth factors, fibrinogen, platelets, whether by the presence of leukocytes or granulocytes, or by the use of an activator.
The first uses of autologous platelet concentrates, the PRF (Platelet Rich Fibrin, total blood without anticoagulant), date back to the 1970s in indications of maxillofacial surgery by Matras H. (2), in the 1980s in the treatment of cutaneous ulcers in the diabetic. The use of this method was widely developed in the 1990s in North America, Asia and Europe, as a surgical adjuvant (3,4,5), to play an important role in sports traumatology for about ten years Years.
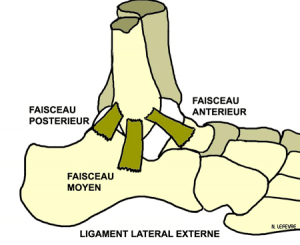
The indications are many, first as surgical adjuvant in the tendinous, bone and ligament repairs, then medical in tendinopathies, ligamentary or muscular lesions and traumatic or degenerative chondropathies like osteoarthritis.
The Executive Committee of WADA(World Anti-Doping Agency ), meeting on September 18, 2010 in Montreal, has withdrawn the use of platelet-derived preparations (PRPs) from the 2011 list.
Scientific basis – mechanism of action
The natural mechanisms of healing on an organism in the case of vascular lesions are the following: activation and platelet aggregation, stabilization of fibrin allowing the formation of a thrombus (clot) and release of growth factors, stimulating cell proliferation and thus The cicatrization .
The principle of PRP treatment is to reproduce these mechanisms of healing and tissue regeneration by injection into the damaged tissue of autologous blood plasma concentrated in platelets. This tissue can be a tendon, a ligament, a muscle, a bone or a joint. The use is purely medical or accompanies a surgical gesture .
The preparation of PRP requires a blood sample , which is centrifuged to separate platelet-poor plasma (PPP, 5%) at the surface, platelet-rich and fibrinogen-rich plasma (PRP, 40%), granulocytes and leucocytes At the bottom of the tube (55%). The cell separator makes it possible to increase the concentration of platelets and growth factors contained in their alpha-granules by 200 to 600%. Depending on the material used and the single or double centrifugation, the composition of the PRP may be variable in terms of platelet concentration and growth factors; It should not contain granulocytes or leucocytes and should not be coagulated.
The use of a local anesthetic before PRP injection is not recommended by the majority of authors, it would modify the local ph, except the PRP is highly dependent.
The platelet-concentrated plasma is then reinjected into the pathological area. These platelets release growth factors in large numbers, allowing the healing of injured tissues by stimulating local stem cells, and reduce inflammation and hemorrhage. The physiopathological hypothesis is that these are Transforming growth factor β and basic fibroblast growth factor (bFGF), which act as humoral mediators to trigger the healing cascade (1). Other factors involved in cell proliferation, differentiation and migration, or in angiogenesis, such as platelet-derived growth factor (PDGF), endothelial cell growth factor (ECGF), platelet-derived PD-EGF Epithelial growth factor), insulin-like growth factor (IGF-I), vascular endothelial growth factor (VEGF) and endothelial cell growth factor (ECGF). TheAlpha granules of the platelets also contain active biological molecules such as serotonin, histamine, dopamine, adenosines, calcium, catecholamines, which play a fundamental biological role in the three phases of repair (inflammation, proliferation, remodeling ). These properties have resulted in a large number of therapeutic indications assess.
Platelet concentrates would have bacteriostatic properties, Highlighted on Staphylococcus epidermidis and Staphylococcus aureus, thus reducing the risk of microbiological contamination of the treated area (Endoret Biotechnology Institute).
NSAIDs should not be used on the previous 10 days and two weeks after the PRP injection, they may inhibit the action of prostaglandins and thus the stimulatory effects of PRP. Local anti-inflammatory care, including the application of cold pockets, should also be avoided. In case of pain, paracetamol will be used.
Graziani ( 20) studied the in vitro action of platelet concentrates on osteoblasts and fibroblasts. He highlighted the stimulatory role of PRP on cell proliferation , particularly sharp at 72 hours, maximum for a platelet concentration of 2.5 times the plasma concentration, higher concentrations reduce this proliferation. This study is an element of response in the choice of platelet concentration to be used in therapeutic protocols. He joinsIn this sense of other authors in particular Weibrich (24).
Gerben M. van Buul (22) studied the effect of platelet concentrates (6x) on human chondrocyte cultures from osteoarthritic knees. Numerous studies have shown the anabolic effects of PRP on the healthy chondrocyte. The interest of this study is to analyze the effect of PRP on degenerative cartilage. The demonstration of an inhibition of inflammatory processesEncourages its use in osteoarthritis.
E. Anitua (23) observed the effect of PRGF (platelet concentrate 2 at 3x) on chondrocytes from arthritic joints. It has demonstrated a stimulatory role on the secretion of hyaluronic acid and angiogenesis.
Publications in osteoarthritis
The use of platelet concentrates in osteoarthritis and chondropathies is of interest to many authors, seeking to clarify their mode of action and compare their efficacy with hyaluronic acid injections or placebo.
Sanchez et al (19) prospectively studied the efficacy of intra-articular injection of PRGF in osteoarthritis in 30 patients compared to a control group of 30 patients treated with intra-articular injection of hyaluronic acid , At the rate of 3 injections at one week interval. They concluded that 33.4% had positive results on pain at 5 weeks in the PRGF group and 10% in the hyaluronic acid group. The beneficial effects at 6 and 12 months were not analyzed, relativizing the interest of this study.
Elizaveta Kon (21) analyzed the efficacy of PRP versus hyaluronic acid in the knee with osteoarthritis or degenerative chondropathy. The analysis3 homogeneous groups of 50 patients treated with either low-molecular-weight HA (AHBP) or By a high molecular weight HA (AHHP), or by PRP. The protocol used consisted in the injection of 5 ml of platelet concentrate (6 ×, anticoagulated and activated), 3 times at 14-day intervals. Patients were assessed by the IKDC score before treatment, at 2 months and at 6 months. The results show a greater and more prolonged efficacy of PRP treatment in more active patients and With less evolved lesions . Results at 6 months of PRP or AH treatment were comparable in older subjects. The authors chose a significantly higher platelet concentration than in Graziani’s in vitro study. The ideal concentration of platelets may not be the same according to therapeutic indications and injection sites.
M. Bouvard and B. Eichene (34 and 35) in 2014 gave an excellent review of the literature on the subject, retaining 6 high-level studies of osteoarthritis, 5 versus AH (28, 29, 30 , 31, 32) And 1 versus placebo (33). The efficacy of PRP is superior to HA or placebo,Especially in patients with early osteoarthritis.
In 2016, Patrick A. Smith (40) in a double-blind, randomized, high-level study investigated the efficacy of placebo- controlled PRP therapy in the knee arthritis (stage 2 and 3 of Kellgren- Lawrence). Of the 114 patients analyzed, 30 were retained in two homogeneous groups, 15 receiving 3 PRP injections and 15 receiving saline (placebo) at 3 injections at one week intervals. TheFunctional repercussion of osteoarthritis was evaluated by the WOMAC score, before and after injection. Patients were monitored for 12 months. The authors do not report any adverse events. The improvement of the 12-month Womac score in the placebo group was 7%, with a 78% improvement in the PRP group , which was felt gradually from the first injection. PRP confirms once again its effectiveness in the treatment of osteoarthritis
Bibliography
1. Iwasaki M, Nakahara H, Nakata K, Nakase T, Kimura T, Ono K. Regulation of proliferation and osteochondrogenic differentiation of periosteum-derived cells by transforming growth factor-beta and basic fibroblast growth factor. J Bone Joint Surg Am 1995; 77: 543-554.
2. Matras H. Fibrin sealant in maxillofacial surgery. Development and indications. A review of the past 12 years. Facial Plast. Surg 1985, 2: 297-313.
3. Proliferation and osteochondrogenic differentiation of periosteum-derived cells by transforming growth factor-beta and basic fibroblast growth factor. J Bone Joint Surg Am 1995; 77: 543-554.
4. Everts PA, Knape JT, Weibrich G, et al. Platelet-rich plasma and platelet gel: a review. J Extra Corpor Technol 2006; 38: 174-187.
5. Marx R GA. Dental and craniofacial applications of platelettrich plasma, 2005.
19.Sánchez M , Anitua E , Azofra J ,Aguirre JJ , Andia I. Intra-articular injection of an autologous preparation for the treatment of knee OA: a retrospective cohort study. Clin Exp Rheumatol.2008 Sep-Oct; 26 (5): 910-3.
20. Graziani F, Ivanovski S, Cei S, Ducci F, Tonetti M, Gabriele M. The in vitro effect of different PRP concentrations on osteoblasts and fibroblasts. Clin. Oral. Impl. Res. 17, 2006, 212-219.
21. Elizaveta Kon, MD, Bert Mandelbaum, MD, Roberto Buda, MD, Giuseppe Filardo, MD, Marco Delcogliano, MD, Antonio Timoncini, MD, Pier Maria Fornasari, MD, Sandro Giannini, MD and Maurilio Marcacci, MD Platelet- Rich Plasma Intra-Articular Injection Versus Hyaluronic Acid Viscosupplementation as Treatments for Cartilage Pathology: From Early Degeneration to Osteoarthritis.
Arthroscopy: The Journal of Arthroscopy and Related Surgery, vol. 27, No 11 (November), 2011: pp 1490-1501
22.Gerben M. van Buul, MD Wendy LM Koevoet, BSc, Nicole Kops, BSc, P. Koen Bos,* MD, PhD, Jan AN Verhaar, MD, PhD, Harrie Weinans, PhD, Monique R. Bernsen, PhD, and Gerjo JVM van Osch,* Z § PhD Investigation performed at Erasmus MC, Rotterdam, the Netherlands. Platelet-Rich Plasma Releasate Inhibits Inflammatory Processes in Osteoarthritic Chondrocytes. The American Journal of Sports Medicine, Vol. 39, No. 11.
23. E. Anitua, M. Sanchez, AT Nurden, M. Zalduendo, M. de la Fuente, J. Azofra and I. Andia. Platelet – released growt factors. The secretion of hyaluronic acid and induce hepatocyte growth factor by synovial fibroblasts from arthritic patients. Rheumatolgy 2007; 46: 1769-1772. October 2007.
28. Giuseppe Filardo1, Elizaveta Kon1 *, Alessandro Di Martino2, Berardo Di Matteo2, Maria Letizia Merli2, Annarita Cenacchi3, Pier Maria Fornasari3 and Maurilio Marcacci2. Platelet-rich plasma vs hyaluronic acid to treat knee degenerative pathology: study design and preliminary results of a randomized controlled trial.
29. Omer Mei-Dan, Michael R. Carmont, Lior Laver, Gideon Mann, Nicola Maffulli, and Meir Nyska. Platelet-Rich Plasma or Hyaluronate in the Management of Osteochondral Lesions of the Talus. Am J Sports Med March 2012 40 534-541; Published online before print January 17, 2012.
30. Sánchez M, Fiz N, Azofra J, Usabiaga J, Aduriz Recalde E, García Guitierrez A, Albillos J, Gárate R, Aguirre JJ, Padilla S, Orive G, Anitua E. A Randomized Clinical Trial Evaluating Plasma Richin Growth Factors PRGF-Endoret) Versus Hyaluronic Acid in the Short-Term Treatment of Symptomatic Knee Osteoarthritis. Arthoscopy. 2012 Aug; 28 (8): 1070-8.
31. Cerza F, Carni S, Carcangiu A, Di Vavo I, Schiavilla V, Pecora A, De Biasi G, and Ciuffreda M. Comparison Between Hyaluronic Acid and Platelet-Rich Plasma, Intra-articular Infiltration in the Treatment of Gonarthrosis. Am J Sports Med. 2012 vol. 40 (12): 2822-2827.
32. Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with Platelet-Rich Plasma Is More Effective Than Placebo for Knee Osteoarthritis: A Prospective, Double-Blind, Randomized Trial. Am J Sports Med. 2013 Jan 8.
33. Say F., Gürler D., Yener K., Bülbül M., Malkoc M. Platelet-rich plasma injection is more effective than hyaluronic acid in the treatment of knee osteoarthritis Acta Chir Orthop Traumatol Cech 2013; 80 (4): 278-283.
34. Bouvard M., Eichene B. Treatment with PRP 1st part: cartilaginous and muscular lesions. Journal of Traumatology of Sport 31 (2014) 113-120.
40. Patrick A. Smith. Intra-articular Autologous Conditioned Plasma Injections Provide Safe and Effective Treatment for Knee Osteoarthritis: An FDA-Sanctioned, Randomized, Double-blind, Placebo-controlled Clinical Trial. Am J Sports Med published online February 1, 2016.
Doctor Yves GUGLIELMETTI. – 24 novembre 2014.