Introduction
This technique of reconstruction of the anterior cruciate ligament plasty involving extra and intra-articular fascia lata was described by Hey-Groves in 1917, modified in 1972 and MacIntosh Jaeger recently. This reconstruction is a technique increasingly practiced for controlling the tibial rotation and rotational jump experienced by the patient and the surgeon objectified by clinical examination.
This lateral grafting used in this technique is called the fascia lata is a transplant with high resistance comparable to other biomechanical transplants used. The fascia lata retains its tibial insertion, which is a natural attachment system and therefore superior to any other system used. This technique has the advantages of not having to levy tendon and therefore the hope of postoperative muscle recovery and normalization of the fastest isokinetic tests.
Surgical technique
1st time: Charge fascia lata
A skin incision is made, it begins opposite the lateral femoral epicondyle and rises along the rear part of the lateral aspect of the thigh of about 6-8 cm. The subcutaneous tissue is lifted off the fascia lata next to the incision and then up to 10 cm and down to Gerdy’s tubercle.
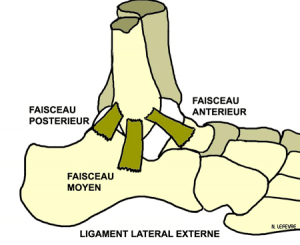
After the exposure of the fascia lata made, plasty will be charged, it should be about 20 cm from Gerdy’s tubercle. To ensure a sufficient width, the two incisions of collection of the plasty flare towards the proximal portion, the posterior incision line must remain parallel to the axis of the thigh, unlike the anterior incision line joining the middle of the lateral side of the thigh. It is important to leave a posterior fascia 1cm about extending this intermuscular septum to a strong closing secondarily. Proximally, the termination of the donor area must be swept allowing easier closing at a finer area and avoiding the risk of muscle hernia. Proximal one will then take off the distal side of the fascia lata vastus then the joint capsule in which there is a separation plane at this level. Distally, identification by palpation of the lateral epicondyle and the lateral collateral ligament (LCL).
2nd time: Preparation of graft
The graft is tubulisée by separate points of resorbable son allowing its passage through the bone tunnels and a continuous suture is accomplished by distally acting tractor wire. Graft calibration of the embodiment which can be of different diameter between the femoral and tibial portion.
3e time: Locating the femoral isometric point of entry
Using a compass, tracking the isometric point for having a graft taut that one is in extension or flexion.
One end of the compass is placed on Gerdy’s tubercle and the other end back and distally with respect to the lateral femoral epicondyle. It is useful to locate the “Lemaire vessels” constant landmarks near the extra-articular isometric area described by Lemaire and Combelles. Several tests are carried out in this area by mobilizing the knee until the isometric points.
Recent studies have shown that isometric item was different from one patient to another depending on their anatomy.
Once found isometric point of the exhibition area electrocautery then obtained from the bone contact, producing a pilot hole in the square tip.
4th time: proximal closure of the fascia
Before time arthroscopic, it is preferable to start the proximal fascial closure, comprising laterally transferring the intermuscular septum, and this for two reasons. The first is explained by the fact that the fascia has not had time to distend the vastus lateralis muscle muscled in some patients is large. The second reason is a control end closing procedure to detect possible weaknesses in this closing wall to strengthen it to avoid secondary muscle hernia wall failure.
5th time: Arthroscopic Time
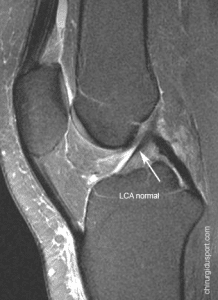
Surgical approaches usual medial and lateral para-patellar common to other plasty. Shaving of Hoffa. The cleaning of the notch is at minimum by keeping the maximum fiber to improve the secondary healing. If one of the beams remain strained fibers, we must of course keep them. Any remainder should be stored but it will thoroughly check the end of the procedure there is no conflict with the roof of the recess or the lateral femoral condyle. The femoral and tibial preparations are classic. First, making the tibial tunnel using the viewfinder set to 55 °, which is identical to other techniques with a ligament intraarticular exit point located between the two tibial spines. Placing the guide wire, check the correct positioning of it then drilling diameter defined during calibration.For the femoral tunnel using a viewfinder “outside-in” whose angle is adjusted according to the found item isometric. Intra-articular exit point of the femoral tunnel is positioned at the posterior part of the medial surface of the lateral condyle. As the tibia, setting up the guide wire, check the correct positioning of this drilling and pre-defined diameter.
Tractors son went inwards in the femoral tunnel and recovered arthroscopically in the notch and at the tibial tunnel. A cycling allows to reach plasty. Finger control checks the tension plasty at the entrance of the femoral tunnel during the transition to the extension confirming satisfactory isometric plasty. Another way to control the isometric is the absence of swallowing plasty on leaving the tibia during extension passage.
Plasty is 30? flex with the foot in neutral rotation. Tibial fixation is achieved by a screw size of interference greater than the size of the transplant. One carries out a final check to see arthroscopic graft and check for any previous conflict at the cut extension.
6th time: Closed
It is very important to release the tourniquet before closing for hemostasis, especially at the Lemaire vessels. Closing begins with the suture of the distal portion of the removal region with interrupted sutures of resorbable son. We must check the end of the procedure the absence of muscle hernia. The skin is closed by an intradermal suture. Most of the time, no drainage is needed if hemostasis was carried out correctly.
Postoperative
They are unremarkable compared to conventional techniques. Support is relieved by two crutches after surgery for several days. A hinged splint will be prescribed for 15 days to lock quadriceps. We recommend a gentle progressive rehabilitation and the first month after the intervention with the aim 0-90 °, recovery of full extension being the first goal.
Doctor Antoine GEROMETTA, Doctor Yoann BOHU, Doctor Nicolas LEFEVRE, Docteur Alain MEYER, Docteur Olivier GRIMAUD, Doctor Serge HERMAN. – 26 février 2016.