The main objective of this study was to present a synthesis of the current literature in order to provide a useful tool for clinicians in radiological analysis of the meniscus. The magnetic resonance imaging (MRI) is the most accurate and least invasive for the diagnosis of meniscal tears. This technique has revolutionized the imaging of the knee and has become the “gold standard” for imaging the meniscus. It confirms and characterize the meniscal lesion, type, extension, its possible association with a cyst meniscal extrusion, assessment of cartilage and subchondral bone. All anatomical descriptions were clearly illustrated in this articleby MRI, arthroscopic and / or drawings. We also described standard radiography for differential diagnosis as osteoarthritis. Ultrasound is often used as a diagnostic tool for meniscal pathology. CT arthrography with multiplanar reconstructions can detect some cracks not visible meniscus on MRI. CT arthrography is also useful in case of against-MRI in the postoperative evaluation of meniscal sutures or for analysis cartilage covering the articular surfaces.
MRI is the most accurate and least invasive method for the diagnosis of meniscal tears.New 3D MRI in three dimensions with isotropic resolution allow creating multiplanar reformatted images to obtain from an acquisition in one sectional plane, reconstructions in other spatial planes. 3D MRI should further improve the diagnosis of meniscal tears
This article describes MRI imaging of all meniscal lesions.
Introduction
The knee arthroscopy is today considered the gold standard in the diagnosis and treatment of intra-articular knee lesions. Preoperative imaging is nevertheless mandatory before any surgical procedures. Indeed the only diagnostic arthroscopy has no place in evaluation of meniscal lesions knee. clinicians (Sports doctor, surgeon or rheumatologist) therefore need to have a precise radiological analysis of meniscal tears (And other lesions) to best fit their treatment.
In the literature, many diagnostic radiological examinations was described for the evaluation of meniscal lesions. But it is the magnetic resonance imaging (MRI) is the most accurate and least invasive for the diagnosis of meniscal tears. This technique has revolutionized the imaging of the knee and has become the “gold standard” for imaging the meniscus. It confirms and characterize the meniscal lesion, type, extension, its association with a cyst meniscal extrusion,assessment of cartilage and subchondral bone. Studies have shown excellent results regarding the sensitivity and specificity of MRI in diagnosing meniscal tears. They allow classify the different meniscal lesions, especially in the early detection of grade I and grade II lesions to reduce the rate of unnecessary diagnostic arthroscopy.
We described the various complementary tests used Today in the diagnosis of meniscal tears with a precise description of all lesions. All anatomical descriptions were clearly illustrated in this articleby MRI, arthroscopic and / or drawings.
Imaging of the menisci
1. Plain radiography:
Conventional radiography is extremely limited in the evaluation of meniscal tears, meniscus is not normally viewed with this type of examination. Plain radiography is not helpful in the research and diagnosis of meniscal lesions. However, conventional radiography of the knee can be requested in case of diagnostic doubt or differential diagnosis such as osteoarthritis, which commonly occurs along the meniscal degeneration. Thus, this examination is recommended in cases of suspected meniscal lesion in the patients over 50 years because of the frequent risk associated with osteoarthritis. A joint space narrowing greater than 50% see a complete pinch can doubt the reality of a possible symptomatic meniscal lesion.
X-rays can also eliminate unexpected injuries, such as osteochondritis or foreign bodies. Finally, in the presence of a discoid meniscus Radiographs may show an enlargement on the compartment concerned in this case most often the lateral compartment.
The X-ray front and profile should be performed in single stance, but also impact schuss to assess and compare the height of the line spacing of the bearing zone compared to the contralateral side.
Radiography can analyze:
- the quality of the bone matrix
- the thickness of the femoral-tibial spaces
- densification of the tibial plateau internal or external
2. Ultrasound:
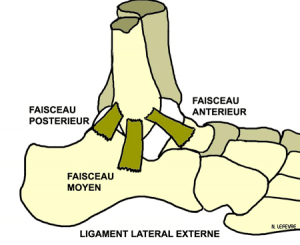
Ultrasonography knee is very useful for the diagnosis of tendon injuries (patellar tendon, quadriceps tendon, tendons of the crow’s feet) and peripheral ligament injury (medial collateral ligament, lateral collateral ligament) (20). Joint effusions (I’hydarthrose or hemarthrosis) and cysts (communicating or not joint) are fine views ultrasound.
However, ultrasound is rarely used as a diagnostic tool meniscal pathology. Although, of Flaviis et al [18] have reported that the dynamic ultrasound has a sensitivity of 82% for the detection of degenerative menisci using criteria based on the meniscal deficiency, cystic lesions or calcifications. Ultrasound can not examine the deep structures of the knee with great precision, more accuracy of ultrasound depends on the skill of the radiologist (operator dependent). The reliability of ultrasound for the diagnosis of meniscal tears is variously estimated in the literature and does not currently seems satisfactory (9,20,31,70). This is not a routine examination in imaging the meniscus. Only meniscal cysts are easily diagnosed and eventually may be aspirated under ultrasound guidance. Rutten et al [70] reported a sensitivity of 97%, a specificity of 86% and an accuracy of 94% in the study of meniscal cysts.
3. Arthrography and CT arthrography
Arthrography knee has long proven its reliability in the diagnosis of meniscal lesions (cracks, bucket handle, meniscal capsular avulsion) with reliability estimated between 83-94% (27,32).
This reference technique in the 70s and 80s, has been completely abandoned in the 2000s in favor of MRI has the advantage of not being invasive examination and to be non-ionizing.
Nevertheless arthrography may be associated with today scanner enabling a arthrography which provides additional information on MRI.
Indeed, thanks to the continuously rotating scanner, achieving spiral acquisition allows for multiplanar reconstructions 2D excellent quality with fine cuts of 0.5 mm.
Reconstructions coronal, sagittal and radial same can detect cracks not visible in MRI, but also capsular meniscal disinsertions by passing the contrast between the meniscal wall and the peripheral capsule. This examinationalso to make a precise analysis of the cartilage of the knee joints and patellofemoral with precise mapping of the lesions. CT arthrography is rarely used in English-speaking countries, but remains a gold standard in the analysis of cartilage with meniscal lesion in Europe. (35)
In the analysis of meniscal lesions, this examination has a sensitivity and specificity between 86% and 100%. The arthrography of the knee is a safe technique that provides accurate diagnosis in identifying meniscal and cartilage damage in patients who can not be evaluated by MRI (Claustrophobia, Pace-maker) or in patients after surgery allowing analysis of meniscal sutures and condition of the cartilage covering the joint surfaces. (19)
4. Magnetic resonance imaging
The magnetic resonance imaging (MRI) is the most accurate and least invasive for the diagnosis of meniscal lesions. This test is more accurate than physical examination and influenced clinical practice and patient care by eliminating unnecessary diagnostic arthroscopy. [37,58,69]
This technique has revolutionized the imaging of the knee and has become the “gold standard” for imaging the meniscus. These benefits analysis in all planes of space meniscal tears, excellent resolution by the sequences allowing a very good analysis of the soft parts. His character allowing parametric based on sequences used to favor viewing such damage or such a structure.
It confirms and characterize the meniscal lesion, type, extension, its association with a cyst meniscal extrusion, assessment of cartilage and subchondral bone. This way, MRI allows an accurate assessment of the stability and the probability of crack propagation. It also determines whether meniscal fissure is repairable or not preoperatively. [56, 68,69, 77]
The advantages of MRI are:
MRI does not expose the patient to ionizing radiation. MRI does not require routine intravenous administration of contrast material, the use of which is sometimes associated with adverse effects. MRI does not require manipulation of the joints. MRI is painless and can be performed in less than 20 minutes.
MRI does not require the intra-articular injection of iodinated radiographic contrast material, unlike the arthrography. arthrography with arthrography has been supplanted by MRI, except for patients who are too large to fit in the MRI unit or for patients who have cons-indications to MRI (eg intracranial aneurysm clips , orbital metallic foreign bodies orPACE MAKER, recent stents). MRI is also useful for the diagnosis of residual or recurrent meniscal tears of the meniscus after surgery. his analysis
The disadvantages or cons indications are:
MRI is limited in patients claustrophobic, obese patients (weight greater than 170 kg) or have a pacemaker. Its usefulness is limited by the presence of artifacts created by the orthopedic nearby. Depending on the implant system used, a variable amount of artifact is observable MRI at the location of fastener material. However, the use of non-ferromagnetic metals such as titanium has reduced the amount of artifact in the postoperative knee (81). Following the use of bioresorbable screws, disturbing artifacts MRI study became much more limited. The added benefit of bioabsorbable screws is all associated artifacts tend to decrease with time. The use of open MRI machines, as well as dedicated end units, decreased the number of patients for whom MRI can not be used because of claustrophobia or obesity. For patients with final against-indications to MRI, computed tomography (CT) during a CT arthrography should be considered as alternative imaging modality.
a. MRI technique
The low MRI machines, medium and high field strength (1, 1.5 or 3 Tesla) can all produce accurate diagnostic images to identify meniscal abnormalities. MRI for low intensity, the number of excitation sequences to be plus for correct meniscal image. This adjustment, however, increases the training time images, and therefore the sequences, which in turn increases the risk of patient movement.Indeed, a small amount of movement can degrade images, compromising the ability to diagnose meniscal tears. [15,80,82]
An antenna specific end (extremity coil) is used to optimize the signal / noise ratio [1]. The lesions of the detection sensitivity of the medial meniscus is comprised between 86 to 96% with a specificity of 84-94%. For the lateral meniscus, the diagnosis sensitivity is from 68 to 86%, and specificity is 92 to 98%. [10,21,24,28,41, 43,59,64,72,73,77] The differences in sensitivity and specificity may be related to sequences used, inter-observer variation, or the sample size . The sensitivity for detection of meniscal tears is generally higher for the medial meniscus regardless of the technique used (60). R Mackenzie et al. (53) describes the overall sensitivity of MRI for the diagnosis of meniscal lesions in 88% with a specificity of 94%. MRI is a widely used1.5 tesla (T) and produces diagnostic images of high quality. There is little data in the literature comparing the musculoskeletal MRI imaging at 1.5T and the 3.0 T. It is expected that the acquisition of faster image at 3.0 T should result in increased accuracy of imaging, or better diagnosis [30,84]. However, Magee et al. (55) established that MRI of the knee performed at 3.0 tesla comparable the sensitivity and specificity studies carried out at 1.5 T. Moreover imaging 3T is not without disadvantage. It increases susceptibility artifacts.
b. Protocols and imaging plane
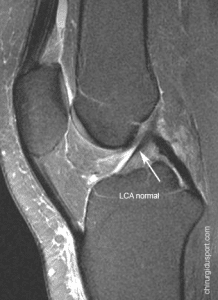
The knee is positioned generally extended with a slight external rotation to facilitate imaging of the anterior cruciate ligament (ACL).
High spatial resolution is needed to show meniscal fissures.
This requires a field of view of about 22 cm (or less), a 3.3 mm slice thickness (or lower). A space of 0.3 mm is used between the image forming sections. A coil end (extremity coil) is used to optimize the signal-to-noise ratio (The signal-to-noise ratio) [8,69,82].
Images must be obtained in the three planes of space sagittal, coronal and axial.
Sagittal images were obtained with the knee in slight external rotation to allow imaging in the plane of the anterior cruciate ligament (indeed, meniscal and ligament injuries are often associated)
Several factors must be considered in the optimization of imaging protocols. Imaging in all three planes is useful, however, all sequences should not be carried out for all plans.
Usually, T1 sequences are performed in the sagittal plane, while T2-weighted images are carried out successively in the 3 spatial planes (sagittal, coronal and axial). [8]
Among the available sequences, we must distinguish anatomical sequences, most pathological sequences. The meniscal structure and meniscal contours are better appreciated on sequences proton density and T2.
- anatomic said sequence: it is mainly the T1-weighted sequences and proton density. MRI of the knee almost systematically include a T1 sequence in the sagittal plane, and to assess the state of the cruciate ligaments, the morphology of the menisci, osteochondral structures of the extensor apparatus (patella, patellar tendon, quadriceps) and the joint cavity.
- pathological sequence known: they are the sequences using the suppression of fat signal whether the STIR or T2-weighted sequences spin echo with specific suppression of the fat signal (T2 and FSE T2 Fat Sat). This sequence is the reference analysis of intra-articular lesions: joint effusions, edematous infiltration, ligament or tendon rupture, bone contusion, bone edema subchondral muscle injury, especially meniscal lesion.
There are other more specific sequences:
- Sequence T1 Fat Sat Gadolinium (T1-weighted sequence with fat-suppressed signal and intravenous gadolinium). This sequence has the advantage of being anatomical but also to be very sensitive on all inflammatory structures and / or vascularized.
- T2 sequence (T2 gradient echo), this sequence little used in other joints (shoulder and ankle) is sometimes used for the knee. His main interest apart from its high sensitivity for the detection of meniscal fissures (63) especially is looking for signs of chronic bleeding in the form of hemosiderin deposits within the framework of villo-nodular synovitis.
Sequences MRI the most reliable for the meniscus are the proton density in sequences (ESF) and T2 sequences Fast spin echo and T2 (11.29) but also sequences in Rho ESF Fat Sat.
c. normal MRI meniscus
A normal meniscus is in the form of a triangular formation of low signal on the T1 and T2-weighted sequences conventional or on the Fast Spin Echo sequence (ESF). The low signal is related to a lack of mobile protons in the normal meniscal fibrocartilage.
In children, a grade 2 signal is often visualized in the posterior meniscal horns. This is considered normal and corresponds to the vasculature of the meniscus of a child. This hyper-signal disappears in adulthood.
d. filing system for meniscal lesions
The MRI semiotics of meniscal fissures is well codified. Using the classification of Stoller and floods in 3 stages [51,79] made proof of its reliability (sensitivity: 87-97% specificity: 89-98%, reliability 88-95% (17, 54). Only abnormalities Stage 3 (hyper linear signal contacting joint) should be retained as pathological.
MRI This classification was developed in correlation with histological pattern. The areas of degenerative lesion shows hyperintensity of varying intensity depending on the location and severity of the meniscal lesion. this classification excludes disinsertions capsular meniscal devices that are considered non-joint. [79]
Grade 1 injury
Grade 1 is a non-articular fissure, focal or diffuse the meniscus. (FIG)
This finding correlates with the early meniscal degeneration.
Terms myxoid degeneration or hyaline degeneration are used interchangeably to describe these lesions.
Grade 2 injury
Grade 2 is a horizontal line image in hyper signal in the body of the meniscus which extends up to the lower surface of the meniscus without crossing it (FIG)
This abnormal signal is wider than in grade 1 but no cleavage or tearing plan is present. Grade 2 progressive degeneration of grade I.
Patients are usually asymptomatic.
Grade 2 signal can be of three types. [79]
- Type 2A is a linear signal without contact articular surface.
- Type 2B is an abnormal signal in contact with the joint surfaces on a single image.
- Type 2C is a very large signal but not in contact with the articular surface. [17, 57]
Grade 3 injury
Grade 3 corresponds to a abnormal signal in the meniscus extending over a large portion of the meniscus and communicating with at least one articular surface of the meniscus. However about 5% of Grade 3 are fissures intra-meniscal without real meniscal cleavage. They may not be diagnosed routine arthroscopy if the extension of the crack on the surface is not identified intraoperatively. [16]
In addition to this description of injuries there are two pathological criteria of meniscal lesions
These two criteria have been established in MRI in diagnosing meniscal tears. If no Prior surgery was not performed on the meniscus, the diagnostic accuracy of meniscal tears is over 90%. [69]
criterion 1
Criterion 1 is a signal alteration in the meniscus consistent with a crack found on at least two consecutive sections; is the concept of “Two-slice-touch rule” with a positive predictive value of 94% of meniscal fissures to the medial meniscus and 96% for the lateral meniscus. The positive predictive value was 55% and 36% for medial and lateral meniscal tears when viewed on one cut. [25,31,69]
The intensity of the abnormal signal should be in contact with a joint surface or the upper surface or inside or at the end (free edge) of the meniscus. If contact with the articular surface occurs on two or more consecutive images, the accuracy of diagnosis of meniscus tear increases. [16,69]
criterion 2
Criterion 2 is concerned with the morphology of the meniscus. A thorough knowledge of normal MRI anatomy of the menisci is required. Meniscal injuries are analyzed on two planes cuts, sagittal and coronal. The visualization of a meniscal fissure on both counts of view reduces the rate of false positive diagnoses. However, a few cracks on the meniscal capsular junction can only be viewed on one of the different planes of cuts.
5. Description of injuries: Sizes, Shapes and Patterns
The representations in multiple section of a meniscal tear must be translated into 3D [68,69]. Meniscal tears occur in both the two main planes: vertical and horizontal. The three forms of meniscus tear base are vertical, radial and horizontal. Meniscal injuries are either partial or total (in all the meniscal thickness)
a. vertical cracks
The vertical cracks are oriented perpendicular to the coronal plane of the meniscus and can be divided into peripheral radial and longitudinal crack crack. They occur most often after a traumatic injury in young patients. [2]
A vertical tear in the thickness of the meniscus contacting the two upper and lower meniscal articular surfaces, completely divides the meniscus into two parts. these crackscan lead to the development of bucket handles [82] The vertical cracks of the posterior horn, may only be visible on sagittal images.
b. radial cracks (or cross)
The radial cracks are vertical lesions and propagating perpendicularly to the main axis of the meniscus. The most common location is the middle segment of the meniscus.The injury begins at the free edge extends a variable distance to the periphery. [82] A complete tear radially extends from the free edge of the meniscus to the periphery (meniscal wall).
Small tears can be difficult to see in MRI. Radial cracks up a large part of the errors in the interpretation of meniscal pathology MRI images. The main feature of the lesion is they involve the free edge of the surface of the meniscus. So, if the inner edge the meniscal triangle coronal is absent or blunted on one or more images, suspect a radial meniscal injuryThese lesions are best seen on sagittal images. (FIG)
The oblique radial lesions (FIG) are a form of radial cracks. They start on the free edge meniscus, then take a longitudinal orientation, similar to longitudinal meniscal tears, the tear extends towards the periphery of the meniscus. The oblique lesions are the most common meniscal tears. [69, 68, 79]
The oblique radial lesions of the posterior horn of the lateral meniscus are often associated with ACL tears. [46]
c. horizontal cracks
cracks horizontal are also called cleavage (cleavage or fish-mouth tears)
They divide the meniscus into two upper and lower portions. They usually start on the underside of the meniscus. [82] Although crackshorizontal may appear deep in the meniscus on MRI, they may extend only a few millimeters arthroscopy. When the lesion extends to the periphery of the meniscus at the menisco-synovial border, they can form a meniscal cyst. Most of his injuries are degenerative, occurring in most patients older with osteoarthritis.
d. complex lesions
Complex lesions can be considered as combinations of Longitudinal lesions, radial, and horizontal.
Several cracks can exist simultaneously within a meniscus, involving different parts of the same region or multiple regions.
Each complex tear of common lesion is composed of a horizontal and radial crack. She is almost always degenerative. [68,69]
e. Avulsion meniscal posterior horn
It is not always easy to make the diagnosis of a meniscal avulsion by MRI. The sensitivity of MRI as a diagnostic tool for detecting the avulsion of the root of the posterior horn is only 66.3%, and is not sufficiently specific to discern the nature of the tear (3) .However, recent studies have helped to improve the sensitivity and specificity of these lesions (4,13,14,22,48,49). Lee et al. (49) proposed a diagnostic assessment based on MRI three signs: the “sign of the ghost” in the sagittal plane (100% detection), the “vertical line defect” (signs of truncation) in the frontal plane (100%), and “radial linear defect” on the axial plane (94%) (FIG)
f. displaced meniscal fragments
The fragments or displaced meniscal tabs occur in 9-24% of meniscal lesions. Any forms of meniscal tear can cause meniscal tabmoved [47] The diagnosis based on MRI visualization of the crack with no meniscal piece and visualization of the meniscal dislocated tongue. [38]
- L’anse Bucket
The bucket handle is the result of a vertical-longitudinal transfixing lesion.
The fragment (dislocated or not) separate meniscal wall, when viewed axially resembles the handle of a bucket. these cracks represent about 10% of all meniscal lesions. [8.38, 39.83] (FIG) The bucket handle lesions (FIG) are diagnosed by MRI, Fragment dislocated in the indentation being seen coronal but also on sagittal sections with search sign double posterior cruciate ligament (PCL dual sign) sagittal section. [16,39,86]
these lesions can be classified into vertical longitudinal single lesion, or not moved, broken or not in the middle part of the meniscus and sometimes double or triple bucket handle. these lesions are three times more frequent in the medial meniscus to the lateral meniscus and may be associated with ACL tears.
The pseudo-hypertrophy of the anterior horn of the lateral meniscus occurs when the anterior horn of the meniscus seems unusually high. The posterior horn of the lateral meniscus is abnormally low. This indicates that a portion of the meniscus tipped forward bucket handle (FIG)
- Languettes meniscal
Meniscal tongues may sometimes move relative to the tilting meniscal body above or below the remainder of the surface of the meniscus. These tabs generally concern the medial meniscus [47]. Displaced tabs infero- medial under the medial meniscus are rare. When the displaced fragment hangs between the peripheral edgethe tibial tray and the part deep medial ligament plan, it may go unnoticed by arthroscopy because the surface of the meniscus may appear intact. However, it is most often visible on coronal MRI (FIG). A vertical tear with a small tab of a segment of a meniscus and moving above or below the meniscal fragment is less common.
g. The meniscal capsular avulsion (Meniscocapsular separation)
The meniscal capsular avulsion is a tearing of the meniscus periphery of the meniscal synovial joint. MRI compared with arthroscopy, is much less reliable for diagnosing meniscal capsular avulsion (positive predictive value: PPV of 9% for the medial meniscus and 13% for the lateral meniscus (67)).
The capsular meniscal is disinsertion frequently associated with ligament injury of the knee. Spontaneous healing is commonbecause of the rich blood supply in the periphery of the meniscus, according to the seat of the avulsion from the connective-vascular area.
h. The meniscal cyst
The meniscal cysts occur more frequently in the medial compartment. [7] The para-medial meniscal cysts are symptomatic and externally because of their location near the medial collateral ligament.The incidence is between 2% and 8%, and these cysts occur most often in men aged 20 to 40 years. The meniscal cysts medial are most often at the posterior horn. [82] While the lateral meniscal cysts are most often located next to the anterior horn of the meniscus.
The cracks are usually horizontal and extend to the periphery of the meniscus, allowing the synovial fluid to escape joint in the para-meniscal soft tissue and forms a meniscal cyst. Sometimes the cyst may be limited to the meniscus. This is called an intra-meniscal cyst.
The para-meniscal cyst located in the anterior horn of the lateral meniscus less likely to have a meniscal tear underlying [23]. It is important to recognize the link between meniscal cyst and meniscal tears. If the cyst is resected without addressing the meniscal tear, the cyst may recur.
i. The meniscal extrusion
The meniscal extrusion of the tibiofemoral joint space has been reported in elderly patients with symptomatic knee OA. In this group, the extrusion of meniscus preceded the development of degenerative joint disease (osteoarthritis) [65]. After extrusion of the meniscus, the direct impingement between the femoral-tibial cartilage majorises progression to osteoarthritis. Lesions of the femoral and tibial cartilage covering, abnormal angulation of the lower limb leading to a disorder of the alignment of the knee, promote meniscal extrusion. Misalignment increase the load transmitted to the surface of the meniscus, which could lead to extrusion. Varus and valgus are respectively associated with a medial and lateral meniscal extrusion. [65]
j. MRI and meniscus surgery
In patients who had a partial resection or meniscal repair, diagnosis of a recurrent tear is more complex, and the use of T2 Fat Sat FSE sequences coronal and sagittal is recommended. Sutured to the meniscus, a hyper linear signal persists at the suture zone, making it difficult differential diagnosis between an iterative crack and a healing way in avulsion (5). If there had resection of more than 25% of the meniscal surface or a meniscal repair, most authors advocate the use of MR arthrography (58). After meniscectomy, the remaining meniscus can present heterogeneous signal and irregular contours without having necessarily a pathological value. The accuracy of MR arthrography in the diagnosis of recurrent meniscal tears was 88%; that of routine MRI is 66%. During extended meniscectomies, the MR arthrography provides more accuracy than simple MRI.
k. The menical discoide (Discoid meniscus)
The differentiation between a real discoid meniscus meniscus and a little larger than normal can be difficult. The three types of discoid menisci are classified as: complete discoid meniscus, incomplete and discoid meniscus Wrisberg.The menisci complete and incomplete discoid vary in their degree of tibial plateau coverage. Wrisberg the variant is less common abnormalities [74].
On sagittal images, discoid meniscus appears as thick bow tie on three consecutive sagittal images. (FIG) The anterior and posterior horns of a normal meniscus are visible on MRI several cuts close to the intercondylar notch. With a discoid meniscus complete, we do not distinguish the difference. The normal meniscus is rapidly shrinking the outer periphery to the center. The presence of a meniscus height of equal or almost equal to 5 mm thick on two adjacent images is a sign of discoid meniscus. [79]
MRI cuts Coronal are most sensitive for the diagnosis of discoid meniscus showing an enlargement of the meniscus. A discoid meniscus may have asymmetric enlargement of the body of meniscus on coronal images, but have anterior horn and posterior normal on sagittal images, stressing the need coronal images. Discoid menisci are correctly diagnosed on MRI (PPV 92%) (71)
l. Stability of the menisci
The meniscofemoral ligaments (Humphry ligament and the ligament Wrisberg) earlier or later are present and visible on 33% of MRI. The Humphry ligament is best seen on sagittal images. It is sometimes observed on the coronal images. The Wrisberg ligament is best seen on posterior coronal images. [70,79,]
6. 3D MRI in three dimensions (3D Isotropic Turbo Spin-Echo MRI)
3D MRI in three dimensions with isotropic resolution has been developed to create multiplanar reformatted images to obtain from an acquisition in one sectional plane, reconstructions in the other plans of the space, seen in the axis of a defined structure as a ligament structure. Besides the visualization of structures in 2D and 3D, this technique also on how to reduce the total duration of the MRI[26,35,36,52,85]. Furthermore, 3D MRI enables visualization of small anatomical structures and can minimize the partial volume effect due to its thin cut. Finally, his field of study may cover the entire area studied without free interval between different cuts [35,44,75]. Thus, MRI 3D has received increasing attention in musculoskeletal imaging because most anatomical structures are small and oriented in various directions, often oblique, particularly in imaging of the ACL (50). Until recently, most 3D isotropic sequences were based on gradient echo imaging (gradient-echo imaging) has drawbacks such as the increased risk of artifact and lack of contrast between normal and pathological tissue[40,87]. Recently, the use of turbo-spin-echo sequences (TSE) allows 3D isotropic image acquisition in a time acceptable scanning [6,34 78]. The knee joint is one of the applications of the most common isotropic 3D sequences. TSE sequence is considered the best sequence for the evaluation of internal structures of the knee due to its High Definition tissue contrast [13, 76]. The TSE sequences of diagnostic performance comparable to MRI spin echo sequences routine, as regards the recovery of cartilage, meniscus, ligaments and subchondral bone [42,45,66]. Recent studies have shown that sequences TSEStandardized even detect a greater number of meniscal lesions and especially the early stages of OA [33, 61].
Conclusion:
The magnetic resonance imaging (MRI) is the most accurate and least invasive for the diagnosis of meniscal tears. This knee of the imaging technique is the “gold standard” of the analysis of meniscal lesions. It confirms and characterize the meniscal lesion. The only diagnostic arthroscopy has So more space in analysis of meniscal lesions knee.
In however, therapeutic arthroscopy is a feasible treatment of meniscal lesions of the knee. The perfect knowledge of different meniscal lesions described in this article allows the clinician to tailor treatment (medical or surgical) specifically to each injury.
New 3D MRI in three dimensions with isotropic resolution should further improve the diagnosis of meniscal tears
Doctor Nicolas LEFEVRE. – 13 mai 2016.