Summary:
Objective: The main objective of the study was to compare the performance of GNRB® and that of Telos ™ in the diagnosis of a partial tear of the anterior cruciate ligament (ACL).
Methods: A prospective study from January to December 2011 included all patients with partial or complete tear of the ACL reconstruction without prior with a healthy contralateral knee. The anterior laxity was measured in all patients by the ™ Télos and GNRB®. The series consisted of 139 patients, mean age 30.7 ± 9.3 years. Arthroscopic reconstruction was performed in 109 patients, 97 for a complete break and 12 uni-fascicular reconstructions for a partial rupture. Conservative treatment wasrecommended 30 patients with partial rupture. The correlation between the two measurement instruments was investigated by Spearman. The optimum threshold values ??of the laximetry were determined using ROC curves and the diagnostic value of the tests was evaluated by the area under the curve (AUC).
Results: The difference between the differential laxity of total and partial tears was highly significant with both tests. The correlation between the two was average laximètres, better between Telos ™ 250N and 250N GNRB® (r = 0.43, p = 0.00001). Analysis of the AUC showed a moderately informative interest for all tests with a better result for the 250N GNRB®: AUC = 0.89 [95% CI from 0.83 to 0.94]. The optimal threshold differential laxity with GNRB® 250N was 2.5 mm (Se = 84%, Sp = 81%).
Conclusion: The diagnostic performance of GNRB® is better than the Telos ™ in Partial ACL tears.

Introduction
The diagnosis of ruptured anterior cruciate ligament (ACL) is clinical. The meta-analysis of Solomon et al [23] showed that the diagnostic test Lachman was the most reliable, followed by the anterior drawer test and the pivot shift test. Nevertheless, objective quantification of the anterior tibial translation is a decision support tool for the surgeon both during the patient’s initial management as for the monitoring. [6] Preoperative differential laxity also gives an indication of the full or partial nature of the break. In case of partial rupture, the therapeutic issue is certain since the conservative treatment can be considered with good long-term results [3,4,7].
Several arthromètres are available [1]. The KT-1000 ™ (MEDmetric®, San Diego, USA) [10] is the most widely used because simple to use. The Rolimeter ™ (Aircast, Summit, USA) is as reliable as the KT-1000 ™ [12,22], but both are examiner-dependent [5,13,17,19]. The Telos ray ™ (Gmbh, Hungen / Obbornhafen, Germany) seems more accurate than the KT-1000 ™ [14]. However this device is expensive and radiating but widely used in Europe preoperatively [9]. Recently available, the system GNRB® (Genourob, Laval, France) showed better reproducibility than the KT-1000 ™ and whatever the level of training of the examiner [8.21].
Pathological laxity are differential thresholds according to the literature 3 mm for the KT-1000 ™ [2.10], 3 mm for the GNRB® [21] and 5 mm for the Télos ™ [24]. In addition, Robert et al [21], in the incomplete ACL tears the threshold value measured at 134 N GNRB® was 1.5mm with a sensitivity of 80% and a specificity of 87%.
The main objective of the study was to compare the performance of GNRB® and that of Telos ™ in the diagnosis of partial ACL tear. The hypothesis of the study was that the diagnosis of GNRB® interest was higher than the Telos ™.
Material and methods
A prospective study was conducted from January to December 2011 in a Sport Surgery service. A local ethics committee agreed.
Criteria for inclusion and exclusion
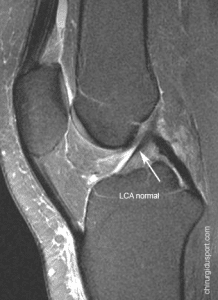
Inclusion criteria were a partial or complete tear of the ACL with a healthy contralateral knee. Exclusion criteria were an old rupture already operated a multi-ligament damage and the patient’s refusal to participate in the study. The diagnosis of clinical failure was confirmed by MRI and measurement laximetry. Conservative treatment was indicated in cases of partial rupture to an absence of pain and knee instability felt by the patient, a scar appearance ACL on MRI and laximetry less than 5 mm in Telos ™ and / or less 3 mm GNRB®. For surgical patients, the rupture was described in part in case of failure of a portion of fiber inspection and ligament remaining taut or total rupture in case of total and / or ligament remaining distended, apparently nonfunctional .
Protocol for Measuring the laximetry
Each patient had a measure of the anterior knee laxity by the Radiation Telos ™ and GNRB® either the same day or a few days apart.
GeNouRoB (GNRB®)
The patient was lying supine on an examination table, the knee in 20 ° flexion and 0 ° of rotation. Each knee was tested compared starting with the healthy knee. A ram exerting pressure of 125N and 250N to the upper part of the calf. The installation of the patient and the handling of the device were performed by a physiotherapist with experience of 2 years on this laximétre. Data were collected on a remote computer Three automated measurements were performed for each pressure and the average of three was chosen. The curves obtained for each knee (anterior tibial translation in mm / thrust force in Newtons) (Fig.1) made ??it possible to automatically calculate one hand the differential laxity and secondly the differential of the slope of the curves, reflecting ligament elasticity [21].
telos ™
The patient was lying on a television radiography table, the knee at 20 ° flexion in the lateral position on the affected side and the healthy side. A thrust 150N 250N was then applied to the proximal portion of the posterior face of the thigh. A radiograph was made ??in this stress position. The measurement of differential laxity was conducted using anatomical landmarks described by Staubli et al, first by a radiology technician trained by the radiologist and the study who had an experience of over 10 years in this unit. In case of discrepancy between the two measures, a third was made.
statistical methodology
The normality of the distributions was tested with the Shapiro-Wilk test. For quantitative variables, if the distributions were normal, parametric tests were used either the Student test. Otherwise, the non-parametric tests were used or the Mann-Whitney test. The correlation between the two measurement instruments was investigated by Spearman correlation coefficient. The optimal thresholds of laximetry with both exams and the slope of the curves in GNRB® were determined through the construction of ROC (Receiver Operating Characteristic) with the x-axis and the y sensitivity (1-specificity). This threshold value was chosen so as to obtain a sensitivity (Se) and a specificity (Sp) the highest possible with the best proportion of subjectshighly ranked. Interest diagnostic tests was evaluated by the area under the ROC curve, AUC (Area Under the Curve): zero (AUC = 0.5), uninformative (0.5 <AUC <0.7) , moderately informative (0,7?AUC <0.9), very informative (0,9?AUC <1), perfect (AUC = 1). [25] A p value less than 0.05 was considered statistically significant.
patients
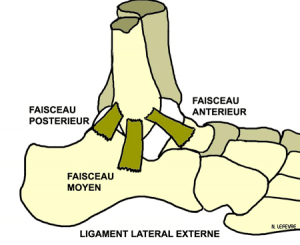
During this period, 139 patients met the criteria of the study population, 84 men and 53 women aged on average 30.7 ± 9.3 years. The accident occurred most often in sport mainly football (29.5%) and skiing (29.5%). Most patients practiced a recreational sport (71%), 26% were competitors and 3% professional athletes. The MRI was performed at a median20 days (1-1588). Measures of laximetry were performed with the devices most often the same day. Arthroscopic reconstruction was performed in 109 patients, 97 ligamentoplasties for a complete break and 12 uni-fascicular reconstructions including 9 anterior-medial and posterolateral 3 for a partial rupture. Conservative treatment was recommended 30 patients with partial rupture.
Results
There was a highly significant difference between the differential laxity of total and partial tears with both exams and whatever coercion. The differential curve slopes at GNRB® was also significantly different depending on the type of failure.
The average correlation was between the two measurement methods, better between Telos ™ 250N and 250N GNRB®.
The ROC curves, differential laxity threshold values ??used for the diagnosis of total rupture was 4 mm (Se = 62.3%, Sp = 73.7%, 66.1% correctly classified subjects) with Telos ™ 150N 3.6 mm (Se = 81.5%, Sp = 59.5% correctly classified 74.6% subjects) with Telos ™ 250N, 2 mm (Se = 83.2%, Sp = 64.3% although classified subjects 77.4%) with GNRB® 125N and 2.5 mm (Se = 84%, Sp = 81%, although classified subjects 83.2%) with GNRB® 250N. The best performance parameters concerned the GNRB® 250N .For the differential between the healthy side slopes curve and the affected side, the threshold value was 2.7 mm / N (Se = 86.3%, Sp = 61.9 % correctly classified subjects 78.8%).
Analysis of different AUC showed that tests all had a moderately informative interest but with a better result for the GNRB® 250N and the differential curve slopes.
Discussion
The main finding of this study was that the GNRB® 250N had a greater interest than the Telos ™ in the diagnosis of partial ACL tears. Both reviews were moderately correlated.
The differential laxity threshold in this study with the GNRB® to 250N was 2.5 mm with a sensitivity 84%, specificity of 81% and allowed to correctly classify over 83% of patients. Robert et al [21], differential laxity threshold value reported GNRB® 134 N in the incomplete ACL tears was 1.5 mm with a sensitivity of 80% and a specificity of 87% and allowed to classify correctly 81 % patients. Reported to the pressure exerted, these parameters are comparable.
Designers GNRB® highlight the interest of the slopes of the differential analysis to evaluate stiffness ligament. [21] In this study, the difference between the partial rupture group and the total breaks this difference was highly significant. On the threshold of 2.7 mm / N, the slope of the differential sensitivity was over 86% with a proportion of correctly classified subjects of almost 79%.
This study also identified a differential laxity threshold in partial ACL tears with Telos ™. With a force of 250N, the threshold was 3.6 mm with good sensitivity (81.5%) but an average specificity (59.5%) exposing a greater number of false positives. The study Osawha et al [18] found the Telos ™ 130N average preoperative differential laxity of 6 ± 2.3 mm for breach of the anteromedial bundle and 4.93 ± 1.73 mm for individual breaking the posterolateral bundle. Several studies have suggested that the Telos ™ would be more appropriate to measure the posterior laxity [16,20] but Lee et al [15] have also shown interest in the measurement of anterior laxity with good reproducibility intra and inter-observer.
The study of Garden et al [14] showed better reliability Telos ™ 150N on the KT-1000 ™ in a population of patients operated on for a torn ACL. However the Telos ™ remains an expensive and radiating examination. Recent studies GNRB® [8,21] showed that the measurements were accurate to the order of 1/10 mm, reproducible and non-operator dependent. Also this device has sensors that take into account the activity of the hamstring muscles which helps avoid false negatives. [14]
This study had some strengths. His prospective helped establish procedures systematized measures. Both laximètres were used in all patients. The study population was large and representative since it was a continuous series of 139 ACL tears, total and partial, operated and non-operated.
However she also had limitations. The main bias was using laximetry as one of the diagnostic criteria for partial tears. Indeed, this diagnosis was based on a set of clinical whose differential laxity, radiological and surgical to surgical patients. There is currently no preoperative examination to ask definite diagnosis of partial rupture [11]. Improving the performance of diagnostic tools for partial ACL tears is a real therapeutic challenge.
Conclusion
The diagnostic performance of GNRB® is better than that of Télos ™ inPartial ACL tears. The differential laxity threshold with GNRB® 250N was 2.5 mm (Se = 84%, Sp = 81%) and the differential slope of 2.7 mm / N (Se = 86%, Sp = 61 9%).
References
1. AHLDEN M, Hoshino Y, K Samuelsson et al (2012) Dynamic knee laxity measurement devices. Knee Surg Sports Traumatol Arthrosc 20: 621-632
2. Bach BR, Warren RF, Flynn WM et al (1990) Evaluation of Arthrometric knees That torn anterior cruciate-have a ligament. J Bone Joint Surg Am 72: 1299-1306
3. Bak K, Scavenius M, S Hansen et al (1997) Isolated partial rupture of the anterior cruciate ligament. Long-term follow-up of 56 squares. Knee Surg Sports Traumatol Arthrosc 5: 66-71
4. Barrack RL, SL Buckley, Bruckner JD et al (1990) Partial versus full acute anterior cruciate ligament tears. The results of nonoperative treatment. J Bone Joint Surg Br 72: 622-4
5. Berry J, Kramer K, J Binkley et al (1999) Error Estimates in novice and expert raters for the KT-1000 arthrometer. J Orthop Sports Phys Ther 29: 49-55
6. Branch TP Mayr HO, Browne JE et al (2010) Instrumented anterior cruciate ligament examination of injuries: Minimizing manual flaws of the clinical examination. Arthroscopy 26: 997-1004
7. Buckley SL, Barrack RL, Alexander AH (1989) The natural history of conservatively biased Treated anterior cruciate ligament tears. Am J Sports Med 17: 221-225
8. Collette M Courville J, M Forton Gagniere B (2012) Objective assessment of anterior knee laxity; comparison of the KT-1000 and GNRB® arthrometers. Knee Surg Sports Traumatol Arthrosc 2012 Jan 10. [Epub ahead of print]
9. Colombet P, Dejour D Panisset JC et al (2010) Current concept of partial anterior cruciate ligament ruptures. Orthop Surg Res Traumatol 96: S109-118
10. Daniel DM, Stone ML, Sachs R, L Malcolm (1985) Instrumented measurements of anterior knee laxity in patients with acute Anterior Cruciate Ligament disruption. Am J Sports Med 13: 401-407
11. DeFranco MJ, Bach BR (2009) A comprehensive review of partial anterior cruciate ligament tears. J Bone Joint Surg Am 91: 198-208
12. Ganko A, Engebretsen L, Ozer H (2000) The rolimeter a new arthrometer Compared with the KT-1000. Knee Surg Sports Traumatol Arthrosc 8: 36-39
13. Huber FE, Irrgang JJ, C Harner, Lephart S (1997) Intratester intertester and reliability of the KT-1000 arthrometer in the assessment of posterior laxity of the knee. Am J Sports Med 25: 479-485
14. Garden C, C Chantelot, Migaud H et al (1999) Low accuracy of KT-1000 versus Telos radiographic measurements for Assessment to anterior knee laxity after-ACL graft. Intra and Interobserver reproducibility of KT-1000. Rev Chir Orthop Reparation on Appar Word 85: 698-707.
15. Lee YS, Han SH, Jo J et al (2011) Comparison of 5 different methods for measuring stress radiographs to Improve reproducibility During the assessment of knee instability. Am J Sports Med 39: 1275-1281
16. Margheritini F, L Mancini Mauro CS, Mariani PP (2003) Stress radiography for Quantifying posterior cruciate ligament deficiency. Arthroscopy 19: 706-711
17. Muellner T Bugge W, S Johansen et al (2001) Inter- and intra-test comparison of the Rolimeter knee test: effect of test’s experience and the technical examination. Knee Surg Sports Traumatol Arthrosc 9: 302-306
18.Ohsawa T, Kimura M, Y Kobayashi et al (2012) Arthroscopic assessment of ligament remnant preserved after-selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy 28: 807-817
19. Papandreou MG, Antonogiannakis E, C Karabalis, Karliaftis K (2005) Inter-rater reliability of measurements Rolimeter entre anterior cruciate ligament and normal contra lateral Injured knees. Knee Surg Sports Traumatol Arthrosc 13: 592-597
20. Pugh L, R Mascarenhas, Arneja S et al (2009) Current concepts in knee-instrumented laxity testing. Am J Sports Med 37 (1): 199-210
21. Robert H New S, S Gageot Gagniere B (2009) A new knee arthrometer, the GNRB: experience in full and partial ACL tears. Orthop Surg Traumatol Res 95: 171-176
22. AJ Schuster, J. McNicholas, Wachtl SW et al (2004) A new mechanical testing device for measuring anteroposterior knee laxity. Am J Sports Med 32: 1731-1735
23. Solomon DH, Simel DL, Bates DW et al (2001) The rational clinical examination. Does this patient-have a torn meniscus or ligament of the knee? Value of the physical examination. JAMA 2861610-1620
24. Stäubli HU, Jakob RP (1991) Anterior knee motion analysis. Measurement simultaneous radiography. Am J Sports Med 19: 172-177
25.Swets JA (1988) Mesuring the accuracy of diagnosis system. Science 240: 1285-1293
Doctor Nicolas LEFEVRE, Doctor Yoann BOHU, Doctor Antoine GEROMETTA, Doctor Shahnaz KLOUCHE , Doctor Serge HERMAN. – 11 janvier 2015.