Introduction
The articulation consists of two major tissues: the articular cartilage and subchondral bone. The cartilage protects the subchondral bone of high stress, shock absorption, distributes the load and facilitates movement. Unlike other tissues, cartilage has very limited capacity of regeneration due to the absence of in-situ vascularization and low capacity of chondrocyte proliferation. At best, the spontaneous healing leads to the formation of a fibrocartilage with biomechanical properties are significantly lower than those of hyaline cartilage.
Cartilage injuries are original or degenerative or traumatic located on bearing areas often in young adults. They are manifested by persistent pain, joint swelling, blockages or collisions and decreased joint mobility. Without treatment, they can progress to osteoarthritis which is particularly problematic in young patients wishing to keep a high level of activity [1].
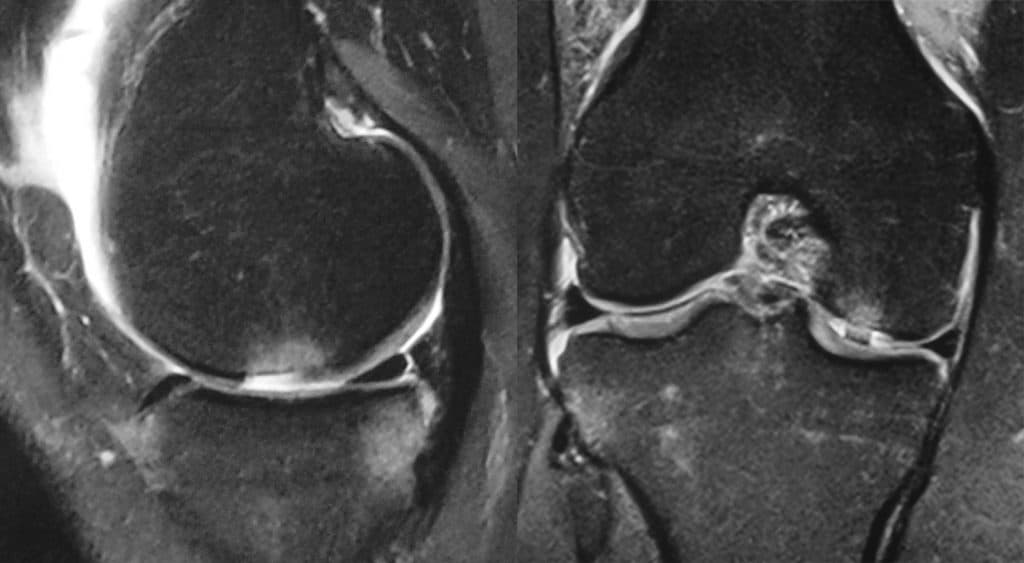
Curl et al [2] have reviewed 31,516 knee arthroscopy and indicated that 63% of
knees showed chondral lesions (mean 2.7 lesions / knee), 20% had complete lesions, 5% in patients younger than 40 years. Sixty-five percent of patients had meniscal or ligament lesions usually a torn anterior cruciate ligament.
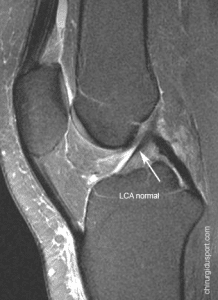
The diagnosis is suspected clinically and on standard radiographs. Arthrography, MRI and MR arthrography possible to assess more precisely the width of the coronal and sagittal length on (Fig 1). Arthroscopy allows an assessment of the depth of the lesions [3]. Several of these lesions arthroscopic classifications have been proposed. The oldest and most widely used is that of Outerbridge because it is easy to use in routine practice [4] (Table 1). The classification of the International Cartilage Repair Society (ICRS) [5] (Table 1) is based on the depth of the lesion.
Treatment options are many. The choice of treatment depends on several factors, mainly the level of activity and the patient’s age, etiology and grade of the lesion.
The purpose of this literature review was to locate the interest of arthroscopic debridement and perforations in the current armamentarium.
treatment options
Conservative treatment
The goal of this treatment is to reduce symptoms and not wound healing. It is essentially of: weight loss, reduction in sports, wearing insoles, partial landfill of the member concerned, the prescription of analgesics and anti-inflammatory, calcium supplementation, see intra-articular steroid injections or visco-supplementation of hyaluronic acid injection. Messner and Maletius [6] published the results in more than 14 years of decline in 28 patients with severe cartilage injury of the knee, not made. Clinical outcomes were considered good to excellent in 22 patients, but the majority of them had radiographic abnormalities in type narrowing of the joint space in the compartment concerned. This treatment is usually attempted in case of small lesions, usually discovered incidentally, at little or no symptomatic patients.
Arthroscopic lavage and debridement
This treatment is to reduce pain and inflammation. Joint lavage usually made ??with saline removes inflammatory cells, mediators of inflammation and cartilage fragments. Debridement additionally allows removal of loose bodies not removed by washing, a limited synovectomy and a regularization of the articular surface. Debridement is often realized with a shaver. Jackson [7] described 45% of sustained improvement over 3 years, 35% of temporary improvement at 15 months after an arthroscopic lavage. When concomitant debridement, the same team showed an immediate improvement in 88% and a sustained improvement in 68% of patients over 3 years [8].
Subchondral stimulation techniques
Different subchondral stimulation techniques have been proposed. They are to mobilize mesenchymal cells from the bone sub-chondra, the capable of differentiating into fibrochondrocytes.
Perforations Pridie
Described by Pridie in 1959 [9], it is to do with fine strands, multiple perforations of the subchondral plate. It is still used today. [10] This technique exposes the risk of local thermal necrosis motorized wicking. Insall [11] in 1974 showed that at 6 years of decline, the success rate was low, on the order of 40%.
Abrasion
This technique first described by Johnson in the 80, is to heighten the subchondral bone for bleeding. This abrasion is done with motorized strawberries on a shaver. Studies have shown that the initial good results have deteriorated over time [12, 13]. This technique was abandoned.
microfractures
Described for the first time by Steadman [14], this technique is performed arthroscopically with specific instrumentation (Fig. 2). This is the reference technique. After debridement of the lesion riverbanks, 3 mm deep perforations are made ??every 3 mm from the periphery to the center. Bleeding must be found through these pinholes. In the postoperative course, if the lesion is in the bearing surface, the support is prohibited for 6 to 8 weeks. Continuous passive motion on arthromotor is started early, 8 hours per day for 8 weeks. [15] Steadman [16] reviewed 71 patients of 73 to a mean of 11.3 years. The average defect cartilage was 2.79 ± 2.14 cm 2. He notes that 86% had normal or near normal function. 43% return without restriction to their sporting level, some 43% and 14% reductions have reduced athletics. Other studies have shown less favorable results with this technique. Miethöfer [17] evaluated 52 patients who underwent the procedure more than 4 years of decline. The average size of the defect was 4.8 cm2. While clinical results as clinically ICRS score was significantly improved in the first 18 months, a deterioration occurred then. Other studies have also shown that initial improvement followed by a marked clinical deterioration [18, 19]. This is explained by the newly formed cartilage composition which is partly fibrocartilage whose biomechanical properties are significantly lower than that of hyaline-like cartilage [20].
Osteochondral autografts by mosaicplasty
This technique performed arthroscopically or open pit, involves removing cylindrical osteochondral grafts at a site not carrying donor then transfer them to the recipients bearing areas wells drilled at the area to be grafted (Fig. 3) . Cylinders of 2.7 to 8.5 mm in diameter and 15-20 mm deep are recommended for this operation. Specific ancillary possible to embed in “press-fit” the collected cylinders. Experimental studies have shown that it is necessary to replace at least 70% of the missing cartilage surface to get a good result. Histological studies both animals and humans [21, 22] showed that approximately 10 weeks after surgery, the transplanted area contained 60 to 70% of hyaline cartilage and 30 to 40% of fibro-cartilage, latter being formed from the previously sharpened cancellous bone. The collection of morbidity is low Hangody et al. [23] reported in a retrospective study of more than 1,000 transplants mosaic, 3% morbidity with four infections and 36 hemarthroses. Arthroscopic checks showed, moreover, that the donor sites were covered with fibrocartilage and remained asymptomatic insofar as it is non-load bearing areas. This technique is widely used in France [10, 24]
osteochondral allografts
These are usually massive transplants. Because of viral risk, allografts are not allowed in France.
Transplant autologous chondrocyte
This technique is used in Sweden since 1987 [25]. The technique is performed in three steps: biopsy, growing chondrocytes and implantation. The healthy cartilage biopsy in non-bearing zone is performed arthroscopically. Chondrocyte in vitro culture is carried out in a laboratory cell culture for 3 weeks. Under arthrotomy, the chondrocyte culture is then injected under a periosteal flap tight previously sewn on the edges of the lesion. An evolution of the technique is to not realize periosteal patch source ossification and cutaways [10] and use a matrix that serves as support for growing chondrocytes [26] (Fig. 4 and 5). Active and passive rehabilitation is carried out for 8 weeks, without support. The sport is taken at 12 months minimum. Several studies have shown the effectiveness of this technique in cartilage defects of the knee [27, 28]. Cohort studies have shown that the clinical and histological results in the medium and long term were excellent, sometimes more than 11 years. However, this technique has its limits: a learning curve, high cost and a significant complication rate. [30] An extensive literature review published in 2010 by Cochrane Library analyzed all randomized trials comparing this technique with other therapeutic options in the treatment of cartilage defects of the knee [31]. The authors concluded that other quality studies, assessing the longer-term results should be conducted before concluding on the efficacy and safety of this technique.
Decision algorithm (Fig. 6)
Recommendations of the High Authority for Health
In 2005, an expert group evaluated autologous chondrocyte transplantation of the knee [32]. This is indicated in patients aged 15 to 50 years, taking into account the level of physical activity, with a loss of symptomatic chondral traumatic unipolar substance, after a non-surgical treatment, and depending on the size of the lesion . Cm2 between 1 and 3: balancing the microfracture, osteochondral autograft in, or autologous chondrocyte implantation; between 3 and 8 cm2: to balance the osteochondral autograft or autologous chondrocyte transplantation and beyond 8 cm2 chondrocyte transplantation is not recommended. Strict cons-indications are: less than 1 cm2 injury, osteoarthritis and total meniscectomy.
Development of the French Society of Arthroscopy on the treatment of cartilage defects of the knee losses in 2010
Only symptomatic and deep lesions (ICRS III and IV) should receive surgical treatment. Osteoarthritis is an absolute contraindication against. The mosaicplasty is the gold standard in France but difficult to achieve. Microfractures are indicated in patients whose functional demand is low. Transplants Autologous chondrocyte be reserved for losses greater than 2 cm 2.
What is the place of the wash-debridement in the treatment of cartilage lesions?
Several studies have shown the sometimes lasting functional improvement by debridement-washing [7, 8]. A study by Donzin et al showed an unexpected element. This study was to compare the efficacy of autologous chondrocyte implantation with that of mosaicplasty. [33] Cartilage lesions were symptomatic and classified stage III or IV Outerbridge, without reaching the subchondral bone. Patients were randomized to two treatment groups six months after initial debridement. Of the 44 selected patients, 14 (31.8%) patients improved by debridement and have not received treatment originally planned. This was probably due to the small size of the lesions. Other comparative randomized studies are underway as the ACTIVE study (UK) that compares the effectiveness of grafting autologous chondrocyte to standard surgical techniques including debridement. This study will end in 2016.
What place arthroscopic perforations in the treatment of cartilage lesions?
In the literature, this technique remains the reference repair surgery. This is a simple, economic and initial results of which are good. For the SFA [10], this technique should be reserved for patients with low functional demand, and in non-symptomatic lesions discovered incidentally .de less than 4 cm2. For HAS, microfractures are an option to consider for lesions of 1 and 3 cm2 [32]. However, note that in case of failure, such surgery can compromise the future success of a chondrocyte transplantation as demonstrated recently Minas et al. [34] This study could jeopardize the status of “standard treatment” microfractures in the evaluation of new treatments.
Conclusion
Despite the recommendations of health authorities and scientific societies, the treatment of cartilage injuries remains controversial. The development of new methods such as gene therapy, will probably result in the future evolution of decision-making algorithms.
Arthroscopic debridement is a conservative surgery, palliative but improves the clinical symptoms. It can be proposed in case of small lesions in symptomatic patients whose functional demand is low.
Microfractures is reconstructive surgery indicated in lesions less than 3cm2. Postoperative rehabilitation is an important part of successful treatment. It currently remains the gold standard for the evaluation of new treatments.
References
[1] Buckwalter JA, Mankin HJ (1998) Articular cartilage degeneration and osteoarthritis, repair, regeneration, and transplantation. Instr Course Lect. 1998; 47: 487-504.
[2] Curl WW, Krome J Gordon ES, Rushing J, Smith BP, Poehling GG (1997) Cartilage injuries: a review of 31.516 knee arthroscopy. Arthroscopy 13 (4): 456-460
[3] Browne JE, Branch TP (2000) Alternative Surgical treatment of articular cartilage for lesions. J Am Acad Orthop Surg 8 (3): 180-189
[4] Outerbridge RE (1961) The etiology of chondromalacia patella. J Bone Joint Surg Br 43: 752-757
[5] Brittberg M, L Peterson (1998) Introduction of an articular cartilage classification. ICRS Newsletter, 1: 5-8.
[6] Messner K, Maletius W (1996) The long-term prognosis for severe damage to weight-bearing cartilage in the knee: a 14-year clinical and radiologic follow-upon 28 young athletes. Acta Orthop Scand 67: 165-168
[7] Jackson RW (1991) Arthroscopic treatment of degenerative arthritis. In: McGinty JB (ed) Operative arthroscopy. New York, Raven Press, pp 319-323
[8] RW Jackson, HJ Marans, Silver RS (1998) Arthroscopic treatment of degenerative arthritis of the knee. J Bone Joint Surg Br 70: 332
[9] Pridie KH (1959) A method of resurfacing osteoarthritic knee joint. J Bone Joint Surg 41B: 618
[10] Versier G, Dubrana F; French Arthroscopy Society (2011) Treatment of knee cartilage defect in 2010. Orthop Surg Traumatol Res; 97 (8 Suppl.): S140-53.
[11] Insall JN (1974) The Pridie debridement operation for osteoarthritis of the knee. Clin Orthop Relat Res. (101): 61-7.
[12] Johnson LL (1986) Arthroscopic abrasion arthroplasty and pathologic historical perspective: present status. Arthroscopy, 2 (1). 54-69.
[13] Bert J, Maschka K (1989) The arthroscopic treatment of unicompartmental gonarthrosis: a five year follow-up study of abrasion arthroplasty arthroscopic debridement and arthroscopic more debridement alone. Arthroscopy; (1): 25-32.
[14] Steadman JR, Rodkey WG, Singleton SB, et al (1997) for technical Microfracture fullthickness chondral defects: technical and clinical results. Oper Tech Orthop 7: 300-4.
[15] Steadman JR, Rodkey WG Rodrigo JJ (2001) Microfracture: technical surgical and rehabilitation to treat chondral defects. Clin Orthop Relat Res. October 2001; (391 Suppl): S362-9.
[16] Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (2003) Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy. 19 (5): 477-84.
[17] Mithoefer K, Williams RJ, Warren RF, et al. The technical microfracture for the treatment of articular cartilage lesions in the knee. A prospective cohort study. J Bone Joint Surg Am 2005 87 (9):. 1911-1920
[18] Kreuz PC, Erggelet C Steinwachs MR, et al (2006) Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy. 22 (11): 1180-6
[19] Steinwachs MR, Guggi T, PC Kreuz (2008) Marrow stimulation techniques. Injury 39 Suppl 1: S26-31.
[20] Frisbie DD, Oxford JT, Southwood L Trotter GW, Rodkey WG, Steadman JR, JL Goodnight, McIlwraith CW (2003) Early events in cartilage repair after-subchondral bone microfracture. . Clin Orthop Relat Res (407): 215-27.
[21] The Hangody, Kish G Kárpáti Z, et al (1997) Technical Autogenous osteochondral graft for the replacing knee cartilage defects in dogs. Orthop Int 5: 1
[22] Hangody L, G Kish, Kárpáti Z, Szerb I <span lang = “EN-GB” style = “line-height: 200%; font-family: ‘A </ body> </ html>
Doctor Nicolas LEFEVRE, Doctor Yoann BOHU, Doctor Shahnaz KLOUCHE , Doctor Serge HERMAN. – 23 octobre 2013.